Researchers and healthcare professionals have long sought to unravel the complexities of Atrial Septal Defect (ASD), a prevalent congenital heart condition that affects individuals worldwide.
Researchers and healthcare professionals have long sought to unravel the complexities of Atrial Septal Defect (ASD), a prevalent congenital heart condition that affects individuals worldwide.
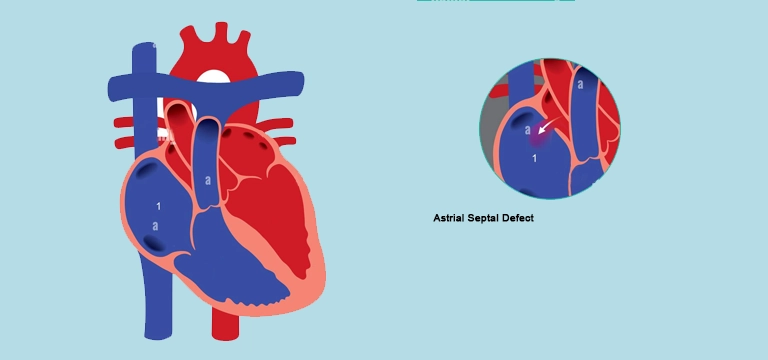
Atrial Septal Defect (ASD) is characterized by an abnormal opening in the septum, the wall separating the heart's upper chambers, leading to blood flow irregularities and potential complications.
With advancements in diagnostic techniques and treatment modalities, the understanding and management of ASD have significantly evolved.
In this article we’ll discuss the intricate aspects of ASD, exploring its causes, diagnostic methods, and treatment options, all aimed at improving patient outcomes and enhancing their quality of life.
Causes & Risk Factors of ASD
There can be several factors that may cause ASD. Let’s discuss them in detail:
Genetic Factors:
- Inheritance patterns indicate a familial predisposition to ASD.
- Mutations or abnormalities in certain genes involved in heart development can contribute to the development of ASD.
- Syndromes such as Down syndrome, Holt-Oram syndrome, and Ellis-van Creveld syndrome have an increased risk of ASD.
Environmental Factors:
- Maternal exposure to certain medications, such as antiepileptic drugs or selective serotonin reuptake inhibitors (SSRIs), during pregnancy, may elevate the risk of ASD in the offspring.
- Maternal consumption of alcohol or tobacco during pregnancy has been associated with an increased likelihood of ASD.
Associated Conditions and Syndromes:
- Down syndrome (Trisomy 21) is commonly associated with ASD.
- Other congenital heart defects, such as ventricular septal defect (VSD) or patent ductus arteriosus (PDA), may coexist with ASD.
- Certain genetic syndromes, including Holt-Oram syndrome (TBX5 gene mutation) and Ellis-van Creveld syndrome (EVC and EVC2 gene mutations), are frequently linked to ASD.
Understanding the causes and risk factors of Atrial Septal defect is vital in identifying high-risk populations and implementing preventive measures. It also underscores the importance of genetic counseling for families with a history of ASD or associated syndromes, promoting early detection and intervention for improved patient outcomes.
Clinical Presentation and Diagnosis of ASD
The clinical presentation and accurate diagnosis of Atrial Septal defects are crucial for appropriate management decisions. Let’s discuss them:
Signs and Symptoms
Many individuals with Atrial Septal Defect (ASD) may be asymptomatic, particularly in cases of small defects. Common symptoms can include fatigue, shortness of breath, and frequent respiratory infections.
Some individuals may experience palpitations or irregular heartbeats. In severe cases, ASD can lead to complications like heart failure or abnormal heart rhythms.
Physical Examination Findings
A thorough physical examination may reveal a distinctive heart murmur, characterized by a "split" or "fixed" second heart sound. The murmur is typically heard best along the left sternal border.
Additional physical signs may include a prominent right ventricular impulse and signs of right-sided heart enlargement.
Diagnostic Tests and Imaging Modalities:
- Echocardiography: It is the primary imaging tool used to diagnose ASD, providing detailed information about the size, location, and characteristics of the defect.
- Transesophageal echocardiography (TEE): It may be utilized in cases where a more accurate assessment is required.
- Electrocardiogram (ECG): Its findings may reveal right Atrial and right ventricular enlargement, as well as other electrical abnormalities.
- Cardiac catheterization: It may be performed to confirm the diagnosis, measure the severity of the shunting, and evaluate the suitability for transcatheter closure.
Timely identification of ASD allows healthcare professionals to provide early interventions, preventing complications and optimizing patient outcomes. A comprehensive evaluation, including a combination of physical examination, imaging modalities, and diagnostic tests, ensures a precise diagnosis and guides the selection of the most suitable treatment approach.
Treatment Options for Atrial Septal Defect
Various treatment options are available for Atrial Septal Defect, considering factors like defect size, location, patient age, symptoms, and overall health. Surgical intervention is recommended for larger defects or cases with coexisting heart abnormalities, involving patching or sewing the defect closed through traditional open-heart surgery.
Minimally invasive techniques, such as video-assisted thoracoscopic surgery (VATS), offer smaller incisions and faster recovery times.
Transcatheter closure is a less invasive procedure, where a closure device is inserted through a catheter to seal the defect. This option is often preferred for smaller ASDs and has shown promising outcomes.
The selection of the most suitable treatment modality is based on careful consideration of individual patient factors and the expertise of the medical team.
The ultimate goal of treatment is to ensure optimal outcomes and improved quality of life for individuals with ASD.
Post-Treatment Care and Complications of Atrial Septal Defect
Post-treatment care for individuals with Atrial Septal Defect focuses on monitoring their recovery, optimizing physical rehabilitation, and vigilant surveillance for potential complications.
Recovery and Rehabilitation:
Following surgical intervention or transcatheter closure, patients may require a period of recovery in the hospital, which can vary depending on the procedure and individual factors.
Physical activity may be restricted initially, with gradual reintroduction under the guidance of healthcare professionals.
Cardiac rehabilitation programs may be recommended to aid in physical conditioning and optimize recovery.
Follow-up Monitoring and Surveillance:
Regular follow-up appointments with cardiologists are essential to monitoring the progress and healing of the Atrial Septal Defect closure.
Echocardiograms and other imaging studies may be performed periodically to assess the effectiveness of the treatment and detect any potential issues.
Ongoing evaluation of heart function, including monitoring for potential arrhythmias or other complications, is crucial in the long-term management of patients with ASD.
Potential Complications and Management:
Complications following ASD treatment can include residual shunting, device-related issues, or the development of other cardiac conditions.
- Residual shunting refers to the persistence of a small opening or leakage after treatment, which may require further intervention or close monitoring.
- Device-related issues can include device malposition, erosion, or thrombosis, which may necessitate additional procedures or interventions.
- The development of other cardiac conditions, such as pulmonary hypertension or arrhythmias, requires appropriate management and treatment.
Regular follow-up appointments and imaging studies allow healthcare professionals to assess the effectiveness of treatment, detect any residual issues, and promptly address complications if they arise.
By providing comprehensive post-treatment care and actively managing potential complications, healthcare teams aim to ensure the best possible outcomes and long-term well-being for individuals with ASD.
Prognosis and Long-Term Outlook of ASD
The prognosis and long-term outlook for individuals with atrial septal defect (ASD) are generally favorable, especially with timely diagnosis and appropriate management. The closure of the defect, whether through surgical intervention or transcatheter techniques, helps prevent complications and improves overall heart function.
With successful closure, individuals can experience a significant improvement in their symptoms and quality of life. Most individuals with ASD can lead normal, healthy lives, participating in regular activities and sports without restrictions.
Long-term follow-up and monitoring are important to detect and manage potential complications, such as residual shunting or the development of other cardiac conditions. By adhering to recommended follow-up care, individuals with ASD can expect a promising prognosis and a positive long-term outlook.
Conclusion:
Early diagnosis and appropriate management are crucial to prevent complications and optimize outcomes.
With advancements in surgical techniques and transcatheter interventions, the treatment options for ASD have expanded, offering patients more choices and improved outcomes.
Long-term follow-up and monitoring are necessary to detect and manage potential complications effectively. By understanding the causes, diagnostic methods, and treatment options, healthcare professionals can provide better care and support to individuals with ASD, ultimately enhancing their quality of life.









