Hemostatic abnormalities, such as bleeding and thrombosis, are frequent side effects that have a significant impact on morbidity and death in cancer patients. (Rodriguez, 2018). The disease process and the use of therapeutic...
A New Study Finds Link Between Bleeding and Thrombosis, Highlighting Importance of Early Detection and Treatment.
Introduction
Hemostatic abnormalities, such as bleeding and thrombosis, are frequent side effects that have a significant impact on morbidity and death in cancer patients. (Rodriguez, 2018). The disease process and the use of therapeutic modalities that might interfere with bleeding or coagulation are two factors that can impact the aetiology of thrombosis and bleeding. (Königsbrügge, Pabinger, & Ay, 2014; Rodriguez, 2014) Among these variables are surgical procedures, chemotherapy, biotherapy, radiation therapy, central venous catheters, supportive care utilising colony-stimulating factors, and newer anticoagulants. By interfering with typical hemostatic processes, a number of tumour- or treatment-related factors, such as changes in platelet function or the coagulation pathway, can raise the risk of bleeding.
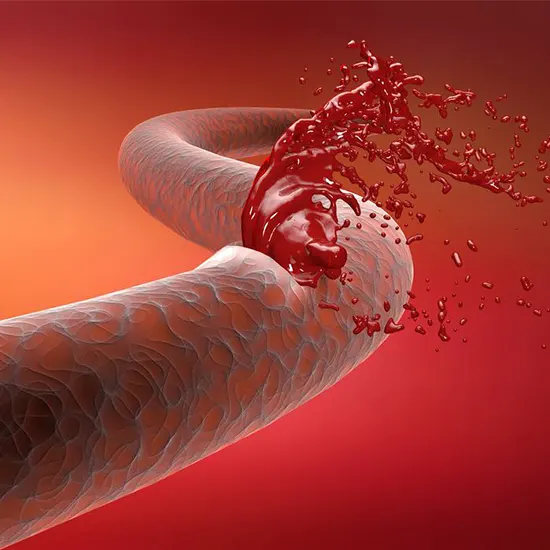
Bleeding
Likewise known as Hematoma, Hemorrhage
When someone bleeds, blood is lost. For example, when you get a laceration or wound, it can be external, or outside the body. Injuries to internal organs are an example of when something is internal, or inside the body. Some bleeding, including gastrointestinal bleeding, blood in the cough, or vaginal bleeding, can be a disease sign.
When you are hurt and begin bleeding, a blood clot typically forms to stop the bleeding fast. The clot then breaks down spontaneously. Your blood requires coagulation factors, which are blood proteins, and platelets, a particular type of blood cell, in order to form a clot. Some individuals struggle with clotting because of a different illness or an inherited disease. There are two distinct kinds of issues:
A bleeding disorder is when your blood does not clot properly. This occurs when your body produces insufficient platelets or clotting proteins, or when they function improperly.
Your blood may clot excessively or the clots may not clear completely.
Bleeding can occasionally result in additional issues. Under the epidermis, a bruise is bleeding. Brain haemorrhage can result in stroke in some cases. First aid or a journey to the emergency room may be necessary for severe bleeding.
What are Some Typical Reasons for Bleeding?
Bleeding is a typical sign. Any number of events or circumstances can result in haemorrhaging. Potential reasons include:
- Haemorrhaging after a trauma
- A wound may result in traumatic haemorrhage. The severity of trauma damage varies.
Typical traumatic injury categories include:
- Bruises or hematomas from abrasions (scrapes) that don't go all the way through the epidermis.
- Lacerations (cuts)
- Puncture incisions caused by objects like knives, nails, or needles
- Devastating wounds
- Bullet holes
- Medical issues
- Some medical problems can also result in bleeding. Less frequently than traumatic bleeding occurs bleeding brought on by a medical problem.
Bleeding can result from the following conditions:
- Haemophilia
- Leukemia
- Hepatic illness
- Menorrhagia, or excessive or protracted menstrual bleeding, is occasionally associated with endometriosis.
- Low blood platelet concentration, von Willebrand disease, and thrombocytopenia
- Vitamin K shortage
- Cerebral injury
- Colorectal cancer lung cancer diverticulosis
- Chronic sinusitis
Medicines
Certain medications and medical procedures can either raise your risk of bleeding or actually cause it. When they initially recommend the treatment, your doctor will inform you of this. They'll also instruct you on what to do if haemorrhaging starts.
The following medicines may be to blame for bleeding:
Blood thinners, when taken for a prolonged period of time, antibiotics, radiation treatment, aspirin, and other NSAIDs
When does bleeding indicate a medical emergency?
If bleeding is excessive, get assistance right away. If you think you might be bleeding internally, you should get assistance right away. This may endanger your safety.
In order to halt bleeding, individuals with bleeding disorders or those taking blood thinners should also seek immediate assistance.
Get emergency attention if:
- The individual has a fever or has gone into shock.
- It is impossible to stop the haemorrhaging by applying pressure.
- A tourniquet is required for the incision
- A severe injury led to the haemorrhaging.
- If the laceration is bleeding, stitches may be required.
- The wound has foreign items stuck inside it.
- Symptoms of an infection include redness, puffiness, or pus leakage that is whitish-yellow or brown.
- Either an animal or a person bit the victim, causing the damage.
As soon as you call for assistance, emergency services will advise you on what to do and when they will appear.
Most of the time, emergency services will advise you to keep applying pressure to the wound and comforting the individual who is bleeding. To lessen their chance of passing out, you might also be instructed to lay the individual down.
How is Haemorrhaging Handled?
In just five minutes, someone can haemorrhage to death. Before help arrives, bystanders might be able to save a life.
Anyone can learn how to stop bleeding thanks to the nationwide Stop the Bleed programme. Even when their injuries shouldn't have been deadly, people in mass casualty incidents have passed away from blood loss.
Emergency Haemorrhage Treatment
Treatment options exist for external traumatic haemorrhage. If you need assistance to stop the bleeding or if the individual is exhibiting any of the above-mentioned emergency signs, call for emergency assistance.
In order to control their heart rate and blood pressure, the bleeding person should attempt to maintain their composure. The speed of bleeding will be accelerated by either a fast heart rate or blood pressure.
To lessen the chance of fainting, lay the person down as soon as you can. Additionally, attempt to elevate the bleeding area.
Remove foreign objects and loose detritus from the wound. Leave bulky objects like knives, arrows, or firearms in their current location. Removing these items might worsen the situation and probably make the haemorrhaging worse. Use pads and bandages to contain the item and stop the haemorrhaging in this situation.
Apply pressure to the area using the following:
- Using a clean cloth, bandage your wrists (after applying protective gloves)
- Till the haemorrhage has slowed and stopped, maintain medium pressure.
- When the bleeding ceases, do not remove the cloth.
- Wrap the dressing around and secure it in position using adhesive tape or clothing. After that, cover the area with a cold pack.
- Inspect the wound to determine whether bleeding has ceased.
- This may disrupt the wound and trigger new bleeding.
- Even if blood seeps through the material, remove the cloth from the incision. Continue applying pressure as you layer on more substance.
- Anyone who has sustained a head, neck, back, or limb injury should be moved.
- To treat an eye laceration, apply pressure
- Only use tourniquets as a very last option.
- The ligature should be applied by an expert.
These actions should be taken to place a tourniquet:
Choose a location for the ligature. Between the haemorrhaging and the heart, apply it to a limb.
If you can, use gauze to create the tourniquet. After wrapping them around the branch, make a half knot. Make sure there is space to make a second knot with the loose ends.
Between the two ties, place a stick or rod.
To secure the bandage, twist the stick.
Using tape or fabric, fix the ligature in position.
Every ten minutes or so, check the ligature. Release the tourniquet and start applying direct pressure if the bleeding has stopped enough to be managed.
What indicates a medical emergency?
You'll require immediate medical attention if:
- Bleeding results from severe damage.
- Haemorrhaging is uncontrollable
- Internal haemorrhage.
- Before bringing you to the hospital, the paramedics will make an effort to stop the haemorrhaging. Care may occasionally be provided on a stretcher or at home. The necessary course of action will rely on what caused the bleeding.
Rarely, haemorrhaging may need to be stopped surgically.
What are the effects of haemorrhaging that is not treated?
Anyone experiencing unexplained or uncontrolled bleeding should be seen by a medical expert.
Haemorrhaging Due to Trauma
Local first aid can halt bleeding if an injury or accident causes it. It might mend on its own if the wound is only minor.
Larger cuts might need stitches, medicated bandages, or corrective surgery.
A medical Haemorrhage
If bleeding is brought on by a medical disease but the condition is not recognised or diagnosed the bleeding is likely to recur.
Without medical attention, any bleeding could become deadly. For instance, someone who experiences acute bleeding rapidly and loses 30% or more of their blood volume may bleed to death very quickly, necessitating IV fluids and a packed red blood cell transfusion for resuscitation.
Thrombosis: What is it?
A blood clot, or thrombus, forming inside of a blood artery is referred to as thrombosis. It hinders the circulatory system's ability to function properly by stopping blood flow.
Any age, color, gender, or ethnicity can be fatally affected by thrombosis.
The body's first line of defence against haemorrhaging is blood clotting, also known as coagulation. Our coagulation system creates a "plug" or "seal" to prevent excessive blood loss when we injure ourselves. After we have healed, our systems frequently dissolve the clot, but occasionally they form improperly or fail to dissolve. A thrombus is a blood clot that develops inside a blood artery and remains there.
Thrombosis:
When a thrombus shapes in a blood vessel
Embolus or Embolism:
A clot that confines and voyages through blood vessels to another portion of the body
There are two primary sorts of thrombosis:
Blood vessel thrombosis alludes to a blood clot that squares a course. Supply routes carry blood absent from the heart to other parts of the body. Blood vessel blood clots can piece bloodstream to the heart and brain, regularly coming about in a heart assault or stroke.
Venous thrombosis, too known as venous thromboembolism or VTE, alludes to a blood clot in a vein. Veins carry blood to the heart from other parts of the body. VTE could be a condition that incorporates profound vein thrombosis (DVT) and aspiratory embolism (PE).
Causes
There are three fundamental causes of thrombosis:
- Hypercoagulability, damage to the endothelial cells of the blood vessel divider and anomalous stream of the blood.
- Hypercoagulability, moreover known as thrombophilia, refers higher levels of coagulation variables within the blood that increment vulnerability to thrombosis. This can be more often than not as a result of hereditary qualities or disarranged of the resistant framework.
- Damage to the epithelial cells on the divider of blood vessels after injury, surgery or and disease can moreover accelerate coagulation and conceivable thrombosis.
- Irregular blood stream, such as venous stasis taking after heart disappointment or long periods of stationary behavior, can moreover cause thrombosis to happen. Also, a few other wellbeing conditions can influence blood stream and lead to the generation of a thrombus, counting atrial fibrillation and cancer.
What are the side effects of blood vessel thrombosis?
Side effects of stroke may incorporate:
- Deadness or shortcoming on one side of your body
- Perplexity
- Slurred discourse
- Hanging mouth
- Inability to lift both your arms
- Sudden vision issue
Side effects of heart assault may incorporate:
- Central, smashing chest torment that transmits to the cleared out bear and arm
- Shortness of breath
- Heart palpitations
- Misfortune of awareness
What are the side effects of venous thrombosis?
Shallow venous thrombosis can cause difficult, ruddy, warm swollen bumps on your leg over and around the site of the clot.
A DVT within the leg or pelvis can cause torment, swelling, redness and warmth within the entire leg, especially within the calf.
Indications of a pneumonic embolism may incorporate chest torment, hacking up blood and trouble breathing. On the off chance that a DVT caused the pneumonic embolism, you'll moreover have indications of a DVT, such as leg torment.
Complications
A common complication of thrombosis is hypoxia, due to the hindrance of the supply route of the vein. When the larger part of the blood vessel is blocked, the oxygen supply to the body is decreased and comes about in expanded generation of lactic corrosive.
Additionally, in some cases the blood clot may break free and travel around the body, a handle known as embolization. This may discourage the bloodstream to basic organs, such as the brain or the lungs, diminishing or restraining oxygen and blood stream with extreme repercussions.
Avoidance and Treatment
As stasis of the blood is related with expanded hazard of thrombosis, it is critical that developments are made frequently, especially in the event that helpless people are likely to be stationary for long periods of time, such as in bed or on a plane.
For individuals with a high chance of venous thromboembolism, heparin can be administered to decrease chance of pneumonic embolism, in spite of the fact related with higher helplessness to dying due to the decreased efficacy of the clotting factors. Subsequently, heparin offers more noteworthy utilisation within the treatment, instead of anticipation of thrombosis.
A more coherent strategy to avoid the arrangement of profound vein thrombosis is the utilisation of compression stockings, which mechanically back the vein to hinder the arrangement of blood clots. This is often especially useful as there are few side impacts.
Anticoagulants may increase the chance of major dying somewhat but have been found to offer an advantage in both the avoidance and treatment of thrombosis.










