Yeasts belonging to the genus Candida are frequently found in both the environment and the human body. There are more than 20 different species of Candida, however, Candida albicans is the most well-known and clinically...
Yeasts belonging to the genus Candida are frequently found in both the environment and the human body. There are more than 20 different species of Candida, however, Candida albicans is the most well-known and clinically significant one.
When Candida species overgrow, they can lead to infections that result in disorders like oral thrush, vaginal yeast infections, and invasive candidiasis, although they are frequently present in tiny numbers in the mouth, gastrointestinal tract, and vagina. Candida infections are more common among persons with weakened immune systems, such as those who have HIV/AIDS or are undergoing chemotherapy, as well as those who have particular medical conditions, including diabetes.
The Diverse Group Of Candida Yeasts That Pose A Growing Threat: Classification of Candida Species.
Candida albicans : The most clinically relevant and often isolated species of Candida is Candida albicans.
Non-Candida albicans
Candida glabrata is an opportunistic pathogen that is becoming more common in medical facilities.
Candida krusei is a rare but dangerous form of invasive candidiasis and candidemia that is inherently resistant to fluconazole, one of the most widely prescribed antifungal medications.
Candida parapsilosis is a diverse yeast that can result in a variety of infections, ranging in severity from moderate to severe and is frequently linked to bloodstream infections brought on by catheter use.
Candida tropical A yeast called Candida tropicalis is being more frequently linked to invasive candidiasis in some areas.
Emerging candida Emerging Candida species are those Candida species that have just lately been recognized as important contributors to candidiasis, such as
Candida auris is an emerging superbug that has caused epidemics in healthcare facilities and is resistant to numerous antifungal medications.
Candida dubliniensis is a yeast that resembles Candida albicans very much but is less usually isolated from clinical samples.
Introduction of Candida albicans
Candida albicans is a kind of yeast that is widely found on healthy people's skin, in their mouths, their guts, and their vagina because it is a typical component of their microbiota. Yet, in some circumstances, Candida albicans can develop into an opportunistic pathogen and cause a variety of illnesses, ranging from invasive candidiasis to superficial skin and mucosal infections.
One of the most prevalent fungal infections in humans, candidiasis caused by C. albicans kills millions of people annually. Vaginal yeast infections, systemic candidiasis, and oral thrush are some of the most typical forms of candidiasis brought on by C. albicans.
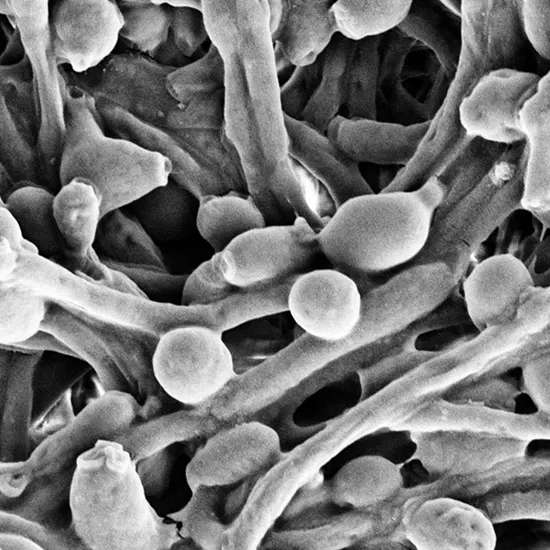
C. albicans can alternate between a single-celled yeast form, a pseudohyphal form, and a true hyphal form, which is a special ability. Its pathogenicity and capacity to spread disease are thought to be strongly influenced by its capacity to transition between several forms.
Although most antifungal medications can successfully treat C. albicans, the emergence of drug-resistant strains is a growing worry. Therefore, it is essential to comprehend the biology and pathogenesis of C. albicans to create fresh methods for preventing and managing the candidiasis brought on by this significant pathogen.
Survival Strategies: The Chlamydospore Form Of Candida albicans.
There are four major stages to the life cycle:
Yeast form : Candida albicans begins its life cycle as an oval-shaped, single-celled yeast cell. At this stage, it can reproduce and divide via budding to create new cells and colonize different parts of the human body.
Pseudohyphal Form : Candida albicans can transform into a filamentous pseudohyphal form when faced with challenges like nutrient scarcity or high temperatures. These cells have grown longer yet are still connected in a chain. It is believed that this form is crucial for attacking host tissues and evading the immune system.
Hyphal Form : The genuine hyphal form, which is a tube-like structure with a branching network of elongated cells, can be assumed by pseudohyphal cells when they come into contact with a suitable environment, such as serum. The hyphal form of the fungus is very invasive and can enter host tissues, allowing it to harm the body and spread throughout.
Chlamydospore Form: Lastly, Candida albicans can develop a latent, thick-walled chlamydospore under specific circumstances, which aids the yeast in surviving unfavorable situations. This form is regarded to be crucial for the fungus' ability to survive in the host and for the emergence of persistent infections.
Itching, Burning, And White Patches: The Uncomfortable Symptoms Of Oral Thrush.
The following list of candida albicans infections' most typical warning signs and symptoms:
Oral thrush : Oral thrush is a common mouth and throat infection that causes white spots to appear on the tongue, inner cheeks, and roof of the mouth. The patches may hurt or burn, and they may bleed if they are scraped. In extreme circumstances, the infection may travel to the esophagus, which would make swallowing painful and difficult.
Genital yeast infection : Candida albicans can also lead to infections in the vaginal region in both men and women. It can result in burning, itching, and a white, thick vaginal discharge in females. It can make the penis of men itchy, red, and irritated.
Skin infection : Candida albicans have been linked to skin infections, particularly in warm, moist places like skin folds. The infection may produce scaling or flaking of the skin as well as a red, itchy rash with tiny pustules.
Nail infection: Candida albicans can also infect the nails, thickening, discoloring, and separating the nail from the nail bed.
Invasive candidiasis : Systemic candidiasis is a severe form of candida albicans infection that can spread to the circulation and other organs. Fever, chills, low blood pressure, and organ failure are possible symptoms.
Candida albicans: A Tricky Diagnosis That Requires Careful Testing.
Clinical Examination : To determine whether a Candida albicans infection is likely, a healthcare professional may do a physical examination and inquire about symptoms. For instance, during a physical examination, the white patches on the tongue and mouth that are present in cases of oral thrush may be seen.
Microscopic Examination : To check for the presence of Candida albicans, a sample of the affected tissue or fluid (such as blood, urine, or vaginal discharge) may be examined under a microscope. The shape and structure of the fungus can be identified using this technique, which can help with diagnosis.
Culture : Candida albicans can be grown under controlled conditions in a laboratory using a sample of the affected tissue or fluid. This approach can assist in identifying the exact Candida species that is causing the infection and identifying which antifungal drugs would be useful in treating it.
Molecular Testing : Candida albicans' genetic material can be found in a sample of infected tissue or fluid using molecular testing like the polymerase chain reaction (PCR). Although not always readily available in healthcare settings, this approach has the potential to be extremely sensitive and specific.
Blood Tests : Blood tests may be carried out in cases with systemic candidiasis to look for indications of infection, such as increased numbers of white blood cells or indicators of inflammation.
What Can Be Treatment Options?
Topical antifungals : For minor skin or nail infections, the affected region may be treated with topical antifungal creams or ointments. Clotrimazole, miconazole, and nystatin are a few examples.
Oral antifungals : Oral antifungal drugs may be administered for more serious or extensive infections. Fluconazole, itraconazole, and voriconazole are a few examples. Depending on how severe the infection is, these drugs are usually taken for a few weeks or months.
Intravenous (IV) antifungal : These may be indicated in patients with severe or systemic candidiasis. Hospitalization may be necessary if these drugs are given straight into a vein.
Lifestyle Modifications : In addition to medicine, lifestyle modifications may be advised to help prevent Candida albicans infections from recurring. Avoiding douching or using scented goods in the genital area, avoiding wearing form-fitting clothing, and practicing proper cleanliness are a few examples.
Always pay attention to your body's signals, and if you think you could have candida overgrowth, consult a doctor.















