When cells mutate and multiply uncontrollably, develop cancer. A lump is formed by the proliferation of abnormal cells known as a tumor. Moreover, neighboring locations can become infiltrated by cancer cells. They can also...
"Breaking the Bonds of Bone: Confronting Chondrosarcoma"
Chondrosarcoma: What is It?
When cells mutate and multiply uncontrollably, develop cancer. A lump is formed by the proliferation of abnormal cells known as a tumor. Moreover, neighboring locations can become infiltrated by cancer cells. They can also spread to different bodily regions.
A bone cancer called chondrosarcoma begins in cartilage cells. The supple connective tissue that borders most joints is known as cartilage. The majority of bones grow from cartilage. Also, it is crucial to the developmental process. There are several distinct forms of cartilage all across the body. The cartilage cells of the shoulder, pelvis, and thighbone (femur) are most commonly affected by chondrosarcoma. Less frequently, it begins in the ribs, skull, knee, and trachea.
The second most frequent primary bone cancer in adults is chondrosarcoma. Every bone cancer that originates from bone cells is considered primary. It differs from cancer which begins in another organ before moving to the bones. This is referred to as bone metastasis or metastatic cancer to the bone.
Epidemiology of Chondrosarcoma
After myeloma and osteosarcoma, primary central chondrosarcoma is the third most prevalent primary bone cancer. The tumor known as chondrosarcoma affects adults and older people. At diagnosis, the majority of patients are older than 50, with a small male predominance. The pelvis, scapula, sternum, and ribs are the axial skeleton bones that are most frequently affected by chondrosarcoma.
Are There Different Types of Chondrosarcoma?
Chondrosarcoma can take various forms:
- Chondrosarcoma with clear cells: Middle-aged men are commonly affected by this form of chondrosarcoma. It frequently appears next to a joint. The growth of chondrosarcomas is typically sluggish, and it rarely metastasizes.
- Chondrosarcoma with no differentiation: Dedifferentiated chondrosarcomas begin as common chondrosarcomas but eventually develop some of the cells of high-grade sarcoma. This particular chondrosarcoma grows more quickly than the majority of other chondrosarcomas and typically appears in older persons.
- Chondromesenchymal tumor: Younger folks are more likely to develop this chondrosarcoma. Compared to other chondrosarcomas, this one frequently develops quickly and is more likely to recur after treatment.
Pathophysiology of Chondrosarcoma
The chromosomal abnormalities 9p21, 10, 13q14, and 17p13 have been identified in several kinds of chondrosarcomas. In well-differentiated chondrosarcomas examined by cytogenetics, anomalies in the structural makeup of the chromosomes and genetic instability have been identified. Moreover, the pathogenesis of chondrosarcoma is significantly influenced by the amplification of the transcription factors MYC and AP-1.
What Causes Chondrosarcoma?
Bone malignancies like chondrosarcoma are currently under investigation for their origins. The hereditary disease Li-Fraumeni syndrome has been connected to chondrosarcoma.
Chondrosarcoma risk is higher for people with specific medical problems such as:
- Maffucci Syndrome( Benign tumor): Hemangiomas, which are knots and befuddlements of surprisingly big blood vessels, are also possible in the form of purplish skin growths in these people.
- The illness Ollier's: These individuals have several benign tumors on their bones, similar to Maffucci syndrome.
- Exostoses Multiplex Heredita (osteochondromatoses): Your bone growth may be hampered by any of these benign bone cancers.
What Chondrosarcoma Signs and Symptoms Are There?
The location and size of the tumor affect the chondrosarcoma symptoms. The following are the most typical signs of chondrosarcoma:
- On a bone, a big bulk
- A sense of pressure surrounding the lump
- Chronic pain that worsens
- A limb or joint that is weak and only partially mobile
- Regional bloating
- Articular stiffness
- Bowel and bladder issues may result from pelvic tumors.
Several of these might be brought on by other health issues. But, if you experience these symptoms, you should visit a doctor. Cancer can only be detected by a medical professional.
Histopathology of Chondrosarcoma
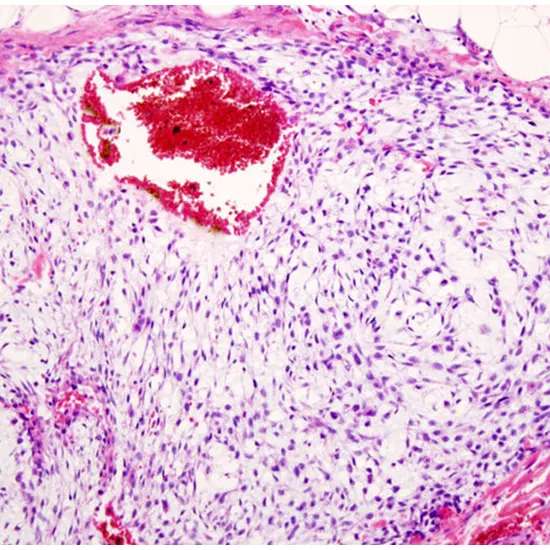
- Macroscopic discoveries: Large tumors, often larger than 4 cm, are chondrosarcomas. They feature a sliced surface that is translucent, lobular, blue-gray, or white, which indicates the existence of hyaline cartilage. There could be spots where myxoid or mucoid material is present, along with cystic alterations. Areas of calcium deposits that are yellow-white and chalky are frequently seen (mineralization). It is possible to see erosion and destruction of soft tissue.
- Microscopic results: Chondrosarcomas produce a lot of the blue-gray cartilage matrix. There are irregularly formed cartilage lobules that range in size and shape. These lobules are divided by fibrous bands or are pervaded by bony trabeculae. There are frequently calcified regions that could indicate the presence of an enchondroma already. The chondrocytes are abnormal, varying in size and shape, and they have larger nuclei that are hyperchromatic. It is common to observe binucleation. Chondrosarcomas frequently exhibit chondroid matrix liquefaction or myxoid alterations. Mitoses and necrosis are visible. With the trapping of bony trabeculae, there is frequent penetration into the cortical bone and the marrow space.
Chondrosarcoma grading is important and helpful in predicting histological behavior.
Based on their histology, chondrosarcomas are categorized into grades:
Grade I: also known as an unusual cartilaginous tumor, this condition is low-grade and locally aggressive. Grade I lesions frequently mimic benign enchondromas or normal cartilage very closely. In this case, distinguishing between benign and malignant tumors frequently hinges on the presence of a "chondrosarcoma permeation pattern," in which the tumor invades the marrow cavity rather than remaining contained by the local architecture. The moderately cellular Grade I chondrosarcoma has hyperchromatic, plump nuclei that are homogeneous in size.
Nuclear atypia hyperchromasia, nuclear size, and cellularity are all more pronounced in grade II malignancies. Mitoses are present.
More pleomorphic and unusual than grade II chondrosarcomas are grade III tumors. Mitoses are simpler to find. Less differentiated and spindly cells are found around the lobules' edges.
Dedifferentiated chondrosarcoma, which accounts for about 10% of all chondrosarcomas, is the fourth type of chondrosarcoma and is regarded as grade IV. Just a tiny percentage of individuals experience dedifferentiation, which is characterized histologically by the presence of a high-grade, frequently spindled, or pleomorphic tumor with little to no cartilaginous matrix. By definition, dedifferentiated chondrosarcoma is a high-grade tumor with a poor prognosis.
Mesenchymal and clear-cell chondrosarcomas are two other, less frequent varieties of chondrosarcomas.
- Immunophenotype: A particular IDH1 R132H antibody can only be used to detect 20% of the IDH1 mutations.
Who is at Risk for Chondrosarcoma?
- Yet, risk factors can increase a person's likelihood of developing cancer. You could have no control over some risk factors. Some, though, might be things you can alter.
- When a person is under the age of 20, chondrosarcoma is uncommon. Age increases risk until about age 75.
- Chondrosarcoma typically begins in healthy cartilage cells. It might also develop from a benign (noncancerous) bone or cartilage tumor.
How to Differentiate Between Osteosarcoma and Chondrosarcoma?
- Osteosarcoma commonly affects children and begins in the bone. Chondrosarcoma commonly affects adults and begins in the cartilage. Healthcare professionals may use surgery alone to treat chondrosarcoma and chemotherapy with surgery to treat osteosarcoma.
- Chondrosarcoma is a dangerous condition. In the spine's bones, it can happen less frequently. Some uncommon types of cancer can be challenging to treat because they grow quickly and are very likely to metastasize.
Evaluation of Chondrosarcoma
- Simple radiography: For the initial assessment, plain radiography is performed. Simple X-rays make it possible to determine the lesion's aggressiveness and cartilaginous composition.
Simple X-rays may provide the following results:
- In 50% of instances, lytic lesions are seen.
- About 70% of the time, intralesional calcifications are present (popcorn calcification or rings and arcs calcification).
- Scaling of the endosteum
- High-grade chondrosarcomas may have a permeative or moth-eaten look.
- Remodeling, thickening, and the periosteal response of the cortex
A Computed Tomography Scan
The following findings can be obtained from a CT scan:
- In 94% of cases, matrix calcification
- Endosteal scalloping
- In approximately 90% of long-bone chondrosarcomas, There is a cortical breach.
- Heterogeneous contrast augmentation
- Magnesium-resonance imaging
When a lesion is lobulated, MRI often shows a high T2 signal intensity and a low or moderate T1 signal.
Sample of Tissue
Chondrosarcoma must be diagnosed and distinguished from other malignant and benign bone tumors via tissue biopsy. Imaging should be used to pinpoint the most aggressive area of the malignancy for biopsy.
Treatment of Chondrosarcoma
The disease's location and the tumors’ level of aggressivity affect the course of treatment. Chondrosarcomas are uncommon, so specialized hospitals with Sarcoma Centers treat them.
The major treatment for chondrosarcoma is surgery. While treating chondrosarcoma, orthopedic oncologists or musculoskeletal tumor specialists are frequently used unless the tumor is in the skull, spine, or chest cavity, in which case a sarcoma-experienced neurosurgeon or thoracic surgeon is preferred. Although amputation is occasionally necessary, it is frequently possible to undertake a procedure that spares a limb. In some circumstances, amputation of the arm, leg, jaw, or half of the pelvis (known as a hemipelvectomy) may be required.
Hemipelvectomy comes in two flavors: internal and exterior.
An external hemipelvectomy involves removing that portion of the pelvis along with amputating the leg.
In an internal hemipelvectomy, the pelvis is removed, but the leg is not affected.
A hip disarticulation is a term used to describe hip amputations, and hip disarms are amputees who have undergone this procedure.
Proton therapy is showing promise with local tumor control at over 80%, although chemotherapy and conventional radiotherapy are ineffective for the majority of chondrosarcomas.
The most effective treatment is complete surgical ablation, however, this can be challenging at times. In difficult areas, proton therapy radiation can be helpful to improve the success of the surgery.
Current research has demonstrated that a viable therapeutic approach for high-grade chondrosarcoma involves inducing apoptosis both directly and indirectly improving response to chemotherapy and radiation.
What Adverse Effects Might a Treatment Cause?
Pain, bleeding, and infection are among the adverse effects that are associated with surgery. However, you will have to deal with the side effects of bone surgery separately. Following surgery, this therapy aids in regaining the damaged area's strength and functionality.
Radiation therapy and other cancer therapies can harm healthy cells. Skin rashes and vomiting are possible side effects of this. Discuss any side effects associated with your treatment with your doctor. To help prevent or control many side effects of treatment, there may be things you can do and medications you can take.
A form of cancer that affects the body's cartilage cells is called chondrosarcoma. It is an uncommon type of cancer that can manifest itself in the bones, ribs, pelvis, and shoulder, among other body areas. Chondrosarcoma comes in a variety of forms, grades, and stages and can be highly difficult.
The following list of chondrosarcoma complications:
- Chondrosarcoma has a strong propensity to metastasize or spread to different areas of the body. It can disseminate to the bones, brain, lungs, and liver. Metastasis can be fatal and result in serious health issues.
- Recurrence: Chondrosarcoma might come back in the same place or other sections of the body, even after successful therapy. A frequent chondrosarcoma consequence that necessitates prompt medical intervention is recurrence.
- Chondrosarcoma can result in excruciating pain and suffering in the affected area. The patient's quality of life may be impacted by the pain, which might be chronic.
- The devastation of bones and joints: Chondrosarcoma can weaken bones and joints, which can result in fractures and dislocations. In extreme circumstances, it may result in irreparable bone and joint damage.
- Disability: Chondrosarcoma can occasionally result in a lifelong handicap. This may be brought on by the breakdown of bones and joints or the amputation of a limb.
- Psychological effects: Patients and their families may have severe psychological effects as a result of chondrosarcoma.
Treatment-related side effects include fatigue, nausea, vomiting, hair loss, and immune system suppression. Chondrosarcoma is treated with surgery, radiation, and chemotherapy.
If you have been diagnosed with chondrosarcoma or exhibit any of its symptoms, you must contact a doctor. The prognosis can be improved and complications can be avoided with early detection and treatment.
Prognosis of Chondrosarcoma
The prognosis is based on how quickly the cancer is identified and treated. 90% of individuals survive more than five years after diagnosis for the least aggressive grade. The survival rate for people with low-grade cancer is typically good. Just 10% of individuals with the most severe grade will live past a year. Future tumor recurrences are possible. Follow-up imaging is crucial for chondrosarcoma treatment.
Dealing with chondrosarcoma can be tough and overwhelming, but it's essential to remember that there are adequate treatments available and to stay optimistic.