A transient ischemic attack (TIA), also commonly referred to as a "mini-stroke," is a temporary disruption of blood flow to a certain part of the brain. It is similar to an ischemic stroke but typically lasts only a...
A transient ischemic attack (TIA), also commonly referred to as a "mini-stroke," is a temporary disruption of blood flow to a certain part of the brain. It is similar to an ischemic stroke but typically lasts only a few minutes and does not cause permanent damage to the brain. TIAs are considered warning signs of a potential stroke, as they share similar underlying causes, symptoms, and risk factors.
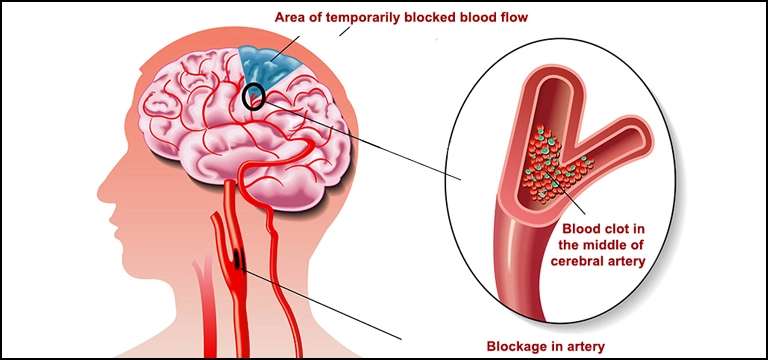
During a TIA, a blood clot or plaque temporarily blocks an artery supplying blood to the brain, leading to a temporary loss of blood flow. The symptoms experienced during a TIA are similar to those of a stroke but usually last for a shorter duration. Common symptoms may include sudden weakness or numbness in the face, arm, or leg (often on one side of the body), difficulty speaking or understanding speech, loss of vision or blurred vision, dizziness, and difficulty with balance or coordination.
It is crucial to take TIAs seriously and seek immediate medical attention, even if the symptoms resolve quickly. Although the effects of a TIA are transient, they indicate an increased risk of a more severe stroke in the near future. Prompt medical evaluation can help identify the underlying cause of the TIA and initiate appropriate preventive measures to reduce the risk of a stroke.
The causes of TIAs are similar to those of ischemic strokes and often involve the formation of blood clots or atherosclerosis (the buildup of fatty deposits in the arteries). Risk factors for TIAs include high blood pressure, smoking, diabetes, high cholesterol levels, obesity, a sedentary lifestyle, older age, a history of previous TIAs or strokes, and certain heart conditions.
Treatment for TIAs aims to prevent future strokes. This typically involves lifestyle modifications (such as quitting smoking, maintaining a healthy weight, exercising regularly, and managing chronic conditions), medication to control blood pressure, cholesterol, and blood sugar levels, and, in some cases, blood-thinning medications. Additionally, doctors may recommend procedures to remove blockages in the arteries or correct underlying heart conditions if necessary.
If you or someone experiences symptoms of a TIA, it is crucial to seek immediate medical attention by calling emergency services. Time is of the essence when it comes to stroke-related conditions, and prompt treatment can significantly reduce the risk of a more severe stroke and its potential complications.
What are the different types of Strokes?
There are primarily two main types of strokes: ischemic stroke and hemorrhagic stroke. Each of them have different causes as described below-
- Ischemic Stroke: This type of stroke is the most common, accounting for about 80% to 85% of all strokes. It occurs when a blood clot or plaque buildup blocks or narrows an artery, reducing or completely cutting off blood flow to a specific part of the brain. Without an adequate blood supply, brain cells in the affected area begin to die.
There are two subtypes of ischemic stroke:
a. Thrombotic Stroke: Whenever one of the arteries supplying the brain gets clogged by a blot clot, this type of stroke happens. The clot usually develops at the site of atherosclerosis (narrowing and hardening of the arteries due to plaque buildup).
b. Embolic Stroke: It happens when a blood clot or other debris forms elsewhere in the body, often in the heart or large arteries leading to the brain. The clot then travels through the bloodstream until it lodges in a smaller artery within the brain, blocking blood flow.
2. Hemorrhagic Stroke: This type of stroke occurs when a blood vessel in the brain ruptures or leaks, leading to bleeding in or around the brain. Hemorrhagic strokes account for about 15% to 20% of all strokes but tend to be more severe and have higher mortality rates than ischemic strokes.
There are two subtypes of hemorrhagic stroke:
a. Intracerebral Hemorrhage: It happens when a blood vessel within the brain ruptures, leading to bleeding and the formation of a clot within the brain tissue. High blood pressure, trauma, blood vessel abnormalities, or the use of blood-thinning medications are common causes.
b. Subarachnoid Hemorrhage: It occurs when there is bleeding into the space between the brain and the thin tissues that cover it (subarachnoid space). This type of stroke is often caused by the rupture of an aneurysm, a weak or bulging spot in an artery.
It's worth noting that a transient ischemic attack (TIA), as mentioned earlier, is sometimes referred to as a "mini-stroke." However, a TIA is not a true stroke but rather a temporary disruption of blood flow to the brain that resolves within a short period, typically within minutes to a few hours.
Does Transient Ischemic Attack require MRI Brain Angiography?
The decision to perform an MRI brain angiography scan (MRA) after a transient ischemic attack (TIA) depends on various factors and is typically determined by the evaluating physician. While not all TIAs require an MRA, it can be a valuable diagnostic tool in certain cases.
The purpose of an MRA is to visualize the blood vessels in the brain and detect any abnormalities or narrowing that could potentially lead to a stroke. It provides detailed images of the blood vessels using magnetic resonance imaging (MRI) technology.
The need for an MRA may depend on the specific circumstances of the TIA and individual patient factors. Here are some situations where an MRA may be considered:
- Recurrent or prolonged TIA: If a person has experienced multiple TIAs or if the symptoms of the TIA lasted for an extended period, an MRA may be recommended to evaluate the blood vessels and identify any underlying vascular abnormalities.
- High-risk factors: Certain risk factors may warrant further investigation with an MRA. These include a history of known blood vessels abnormalities, such as an aneurysm or arteriovenous malformation, or the presence of significant risk factors for stroke, such as severe atherosclerosis or carotid artery disease.
- Younger individuals: TIAs in younger individuals are relatively rare and may prompt the need for additional investigation, including an MRA, to explore potential underlying causes.
- Uncertain diagnosis: In some cases, the symptoms experienced during a TIA may be atypical or not clearly indicative of a transient ischemic attack. In such situations, an MRA may be performed to rule out other possible causes of the symptoms.
It's important to note that the decision to perform an MRA or any other diagnostic test is made on an individual basis, taking into consideration the patient's specific circumstances and medical history. The evaluating physician will assess the need for further imaging based on the clinical presentation, risk factors, and overall evaluation of the patient.
Conclusion
In conclusion, we have discussed important information regarding transient ischemic attacks (TIAs) and the different types of strokes. A TIA is a temporary disruption of blood flow to the brain, often referred to as a "mini-stroke," and serves as a warning sign for a potential stroke. It shares similarities with ischemic strokes but typically resolves within a short period and does not cause permanent brain damage.
Ischemic strokes, the most common type, occur when a blood clot or plaque narrows or blocks an artery supplying blood to the brain. Hemorrhagic strokes, on the other hand, result from a ruptured blood vessel in or around the brain, leading to bleeding. Both types of strokes have distinct causes, characteristics, and treatment approaches.
While not all TIAs require an MRI brain angiography (MRA), it may be considered in specific situations, such as recurrent or prolonged TIAs, high-risk factors, younger individuals, or cases with an uncertain diagnosis. The decision to perform an MRA is made on an individual basis, taking into account various factors and determined by the evaluating physician.
Prompt medical attention and evaluation are crucial in the case of TIAs or stroke symptoms. Timely diagnosis and appropriate management can help prevent more severe strokes and their potential complications. It is essential to be aware of the risk factors, adopt a healthy lifestyle, and follow medical advice to minimize the risk of strokes.
Never try to replace the information provided here with professional medical advice. If you or someone experiences symptoms of a TIA or stroke, it is important to seek immediate medical assistance by contacting emergency services. Stay informed, be proactive about your health, and take necessary steps to reduce the risk of stroke-related conditions.









