Infectious enterocolitis is a common cause of the condition, and bacterial infections are the most frequently reported. Some of the most common bacterial agents include Escherichia coli, Salmonella, Shigella, Campylobacter,...
“Empowering You To Overcome Enterocolitis And Reclaim Your Health.”
Help Us Put an End On Enterocolitis - Introduction
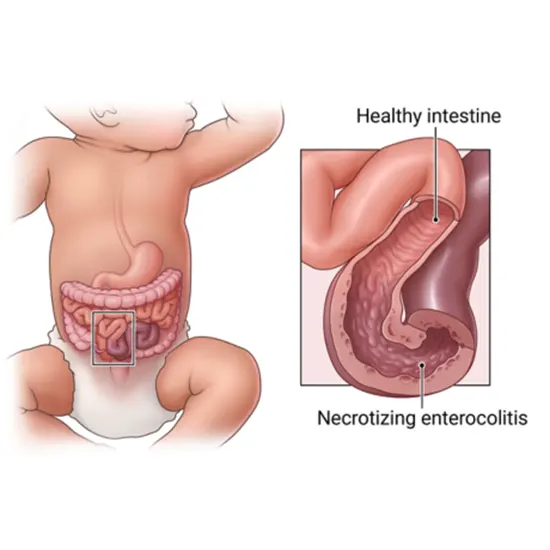
Enterocolitis is a medical condition that causes inflammation of the small intestine and colon
It is typically caused by an infection, either from a bacterial or viral source, which further causes a range of manifestations such as abdominal pain, diarrhea, nausea, vomiting, and fever.
The condition can be acute, meaning it lasts for a short period and resolves on its own, or chronic, meaning it persists over a longer period and requires ongoing treatment.
Enterocolitis can be a serious condition, especially in vulnerable populations such as young children, the elderly, or people with weakened immune systems.
Get Informed About The Dynamics Affected By This Condition - Epidemiology
The epidemiology of enterocolitis can vary depending on the specific cause of the condition. However, some general patterns and trends can be observed.
Infectious enterocolitis is a common cause of the condition, and bacterial infections are the most frequently reported. Some of the most common bacterial agents include Escherichia coli, Salmonella, Shigella, Campylobacter, and Clostridium difficile. Viral infections such as norovirus and rotavirus can also lead to enterocolitis.
Enterocolitis can affect individuals of all ages, but certain populations may be at higher risk. Infants and young children are more vulnerable due to their immature immune systems and may experience more severe symptoms than adults. Older adults and individuals who have depleted resistant systems, such as those with HIV/AIDS or undergoing chemotherapy, may also be at increased risk for enterocolitis.
The incidence and prevalence of enterocolitis vary by geographic location and socioeconomic status. Enterocolitis is more common in countries that have poor sanitation and hygiene practices and may lead to more severe outcomes. In developed countries, enterocolitis is typically less common but can still be a significant health issue, particularly in a hospital or long-term care setting.
Overall, the epidemiology of enterocolitis highlights the importance of proper hygiene practices, timely diagnosis and treatment, and appropriate management of the underlying cause of the condition.
From Cause To Effect Understand The Pathogenesis Of This Condition
The pathogenesis of enterocolitis involves several factors, including the infectious agent, host factors, and environmental factors.
- Some agents such as bacteria or viruses can cause enterocolitis by invading the lining of the small intestine and colon, causing inflammation and damage. These agents may be introduced through contaminated food or water, or contact with infected individuals or surfaces.
- Host factors such as age, immune status, and underlying medical conditions can also play a role in the development and severity of enterocolitis. For example, infants and young children may have immature immune systems that are more susceptible to infections, while older adults or individuals with weakened immune systems may have a reduced ability to fight off infections. There are certain medical conditions such as inflammatory bowel disease (IBD) which may also increase the risk of enterocolitis.
- Environmental factors such as poor sanitation, contaminated food or water sources, and crowded living conditions can also contribute to the development and spread of enterocolitis. In some cases, enterocolitis outbreaks may occur in institutional settings such as hospitals or long-term care facilities, where close contact between individuals and compromised hygiene practices can facilitate the spread of infectious agents.
- Once enterocolitis is established, the inflammatory response can lead to a range of symptoms including abdominal pain, diarrhea, nausea, vomiting, and fever. In severe cases, complications such as dehydration, electrolyte imbalances, and sepsis may also occur.
Overall, the pathogenesis of enterocolitis is complex and multifactorial and involves the interaction of infectious agents, host factors, and environmental factors. Proper prevention and management strategies are essential to mitigate the impact of this condition.
Different Types Of Enterocolitis
Enterocolitis can be classified into different types based on various factors, including the cause, duration, and severity of the condition.
- Infectious enterocolitis: Bacteria, viruses, or parasites are responsible for this type of enterocolitis. Symptoms can range from mild to severe and may include abdominal discomfort, trots, sickness, puking, and fever. Treatment may include antibiotics, antiviral medications, or supportive care criteria such as fluid and electrolyte replacement.
- Antibiotic-associated enterocolitis: This type of enterocolitis is caused by the use of antibiotics, which can disrupt the normal gut microbiota and lead to the overgrowth of pathogenic bacteria such as Clostridium difficile. Symptoms can include diarrhea, abdominal pain, fever, and in severe cases, pseudomembranous colitis. Treatment may involve discontinuing the antibiotic and using probiotics or fecal microbiota transplantation.
- Ischemic enterocolitis: This type of enterocolitis is caused by reduced blood flow to the intestines, which can lead to inflammation and damage to the intestinal lining. Symptoms may include abdominal pain, bloody diarrhea, and vomiting. Treatment may involve restoring blood flow to the intestines and supportive care criteria such as fluid and electrolyte replacement.
- Inflammatory bowel disease (IBD)-associated enterocolitis: This type of enterocolitis is associated with underlying conditions such as Crohn's disease or ulcerative colitis. Symptoms may include abdominal pain, diarrhea, and weight loss. Treatment may involve medications to manage the underlying IBD and to control inflammation.
- Idiopathic enterocolitis: This type of enterocolitis has no known cause and is characterized by symptoms such as abdominal pain, diarrhea, and vomiting. Treatment may involve supportive care measures such as fluid and electrolyte replacement, dietary modifications, and medications to manage symptoms.
What May Be Different Causes?
Enterocolitis can have various causes, which can be broadly classified into infectious and non-infectious causes:
- Infectious causes of enterocolitis are the most common and are typically due to bacterial, viral, or parasitic infections. The most common bacterial causes of enterocolitis include Escherichia coli, Salmonella, Shigella, Campylobacter, and Clostridium difficile. Viral infections such as norovirus, rotavirus, and adenovirus can also cause enterocolitis. Parasitic infections such as Giardia and Cryptosporidium can also lead to enterocolitis.
- Non-infectious causes of enterocolitis are less common but can furthermore help in the development of the condition. Some of these causes include inflammatory bowel disease (IBD), medication side effects, ischemia (reduced blood flow to the intestines), radiation therapy, and autoimmune conditions such as celiac disease.
- Other factors such as a weakened immune system, malnutrition, or exposure to toxins can also increase the risk of developing enterocolitis.
Understanding Symptoms Is the First Key To Recovery - Signs and Symptoms
Some of the most common symptoms of enterocolitis include:
- Abdominal pain and cramping: This is one of the most common symptoms of enterocolitis. The discomfort may vary from soft to painful and may be accompanied by cramping.
- Diarrhea: Diarrhea is another common symptom of enterocolitis. The stool may be loose, watery, or contain blood and mucus.
- Nausea and vomiting: Some individuals with enterocolitis may experience nausea and vomiting, particularly if the condition is severe.
- Fever: A fever may be present in some cases of enterocolitis, particularly if the condition is caused by an infectious agent.
- Dehydration: Diarrhea and vomiting can lead to dehydration, which further leads to symptoms such as dry mouth, fatigue, and decreased urine output.
- Weight loss: Prolonged enterocolitis may lead to weight loss, particularly if the person is not able to eat food normally.
- Abdominal tenderness: The abdomen may be tender to the touch in some cases of enterocolitis, particularly if the condition is causing inflammation.
- Other symptoms: Other symptoms may include bloating, gas, and fatigue.
Different Risk Factors Include
Risk factors for enterocolitis include:
- Age: The age groups which are more susceptible to enterocolitis are infants, young children, and elderly people due to their weaker immune systems.
- Poor hygiene: Some poor hygiene methods, like not washing hands properly before preparing or consuming food, can increase the risk of enterocolitis.
- Depleted immune system: The public with lower immune systems, such as those with HIV/AIDS or who are undergoing chemotherapy, are at increased risk of developing enterocolitis.
- Use of antibiotics: Antibiotics help to imbalance the natural balance of bacteria in the intestines, which can lead to enterocolitis.
- Inflammatory bowel disease: People with inflammatory bowel disease, such as Crohn's disease or ulcerative colitis, are at higher risk of developing enterocolitis.
- Foodborne illness: Eating contaminated food, such as raw or undercooked meat, poultry, or seafood, can lead to enterocolitis.
- Travel: Traveling to areas with poor sanitation and hygiene practices can increase the risk of enterocolitis.
- Malnutrition: Malnutrition, especially in developing countries, can weaken the immune system and increase the risk of enterocolitis.
- Chronic constipation: Chronic constipation can lead to an overgrowth of harmful bacteria in the intestines, which can cause enterocolitis.
- Invasive medical procedures: Invasive medical procedures, such as surgery or colonoscopy, can increase the risk of enterocolitis as there can be a disruption of the biological equilibrium of bacteria in the intestines.
Detecting Early For Better Outcomes - Diagnosis
The following are some common methods used to diagnose enterocolitis:
- Medical history: The healthcare provider will obtain a detailed medical history, which will include questions about the onset and duration of symptoms, recent travel, exposure to contaminated food or water, medication use, and medical conditions.
- Biological Examination: Your physician will conduct a physical examination, which may include abdominal palpation to check for tenderness, bloating, or distension.
- Stool sample analysis: A stool sample may be collected and analyzed to look for the presence of infectious agents which includes bacteria, viruses, or parasites.
- Blood tests: Blood tests may be performed to check for signs of infection, inflammation, or dehydration.
- Imaging tests: Imaging tests such as abdominal X-rays, CT scans, or ultrasounds may be ordered to look for signs of inflammation, bowel obstruction, or other abnormalities.
- Endoscopy: This is a method that involves inserting a flexible tube with a camera into the digestive tract that helps to look for signs of rash, bleeding or other abnormalities.
Healing Is Possible With the Right Treatment
The following are some common methods used to treat enterocolitis:
- Electrolyte and fluid relief: Fluids and electrolytes that are lost through diarrhea and vomiting are essential to replace in treating enterocolitis. This may involve drinking oral rehydration solutions or receiving intravenous fluids in severe cases.
- Antibiotics: Antibiotics may be prescribed in cases of bacterial enterocolitis to eliminate the underlying infection. However, antibiotics are not effective for viral or parasitic enterocolitis.
- Antimotility agents: Antimotility agents such as loperamide or diphenoxylate may be used to reduce diarrhea and associated symptoms. However, these medications should be used with caution in cases of bacterial enterocolitis as they can prolong the infection.
- Probiotics: Probiotics may be used to restore the normal gut microbiota in cases of antibiotic-associated enterocolitis or to reduce the risk of recurrent infections.
- Supportive care: Supportive care measures such as rest, a bland diet, and avoidance of certain foods or substances that may aggravate symptoms may be recommended.
- Surgery: In severe cases of enterocolitis surgery is necessary such as those associated with bowel obstruction or perforation.
What Is the Prognosis Of This Condition?
The prognosis of enterocolitis can vary widely depending on several factors, including the severity and duration of the inflammation, the underlying cause of the condition, and the age and overall health of the affected individual.
In general, mild cases of enterocolitis can often be effectively treated with antibiotics, fluid and electrolyte replacement, and supportive care, and individuals with mild cases can typically expect to make entire healing within a few days to a week.
However, more severe cases of enterocolitis can lead to complications such as dehydration, sepsis, and organ failure, and can be life-threatening if not promptly and effectively treated. In these cases, the prognosis may depend on the underlying cause of the enterocolitis, the severity of the complications, and the speed and effectiveness of the medical intervention.
Overall, individuals with enterocolitis need to seek medical attention and adhere closely to their treatment plan to improve their chances of a positive outcome.
What If Left Untreated?
Some of the most common complications associated with enterocolitis include:
- Dehydration: Prolonged diarrhea and vomiting can lead to dehydration, which may further lead to symptoms such as dry mouth, fatigue, and decreased urine output.
- Electrolyte imbalances: Dehydration can lead to imbalances in electrolytes such as sodium, potassium, and chloride, which can cause symptoms such as muscle cramps, weakness, and irregular heartbeat.
- Malnutrition: Prolonged enterocolitis may lead to malnutrition, as the patient can't diet properly.
- Septicemia: Enterocolitis can lead to septicemia, which is a life-threatening condition that occurs when the infection spreads to the bloodstream.
- Bowel perforation: In severe cases, enterocolitis can lead to bowel perforation, which is a rupture in the wall of the intestine. This can lead to sepsis and require emergency surgery.
- Inflammatory bowel disease: Prolonged or recurrent episodes of enterocolitis can increase the risk of developing inflammatory bowel diseases (IBD), such as Crohn's disease or ulcerative colitis.
Tackling enterocolitis head-on









