Although other bacteria, including Streptococcus or other anaerobic gram-negative bacteria, such as other fusobacteria, can also be connected to this illness, Fusobacterium is frequently involved in the development of...
Although other bacteria, including Streptococcus or other anaerobic gram-negative bacteria, such as other fusobacteria, can also be connected to this illness, Fusobacterium is frequently involved in the development of Lemierres syndrome.In this genus, F. nucleatum and F. necrophorum are the most often isolated species.
However, when the infection is linked to an oropharyngeal abscess, Fusobacterium can cause septic thrombophlebitis in the nearby neck arteries. Fusobacterium are typically found as part of the normal oral, gastrointestinal, and vaginal flora. Infections during pregnancy, bacteraemia, septic shock, and abscess formation are just a few of the possible clinical manifestations.
There are many different clinical characteristics associated with bacteraemia, according to reputable studies on Fusobacterium which found an annual incidence of 0.55 cases per 100,000 people.
Lemierre's syndrome, sepsis in healthy patients, puerperal infections, and sepsis in patients with underlying diseases were the four categories into which the infections were divided by Nohrström et al.in an effort to discover risk factors, comorbidities, and predisposing variables for favourable outcomes.
They stated that various concomitant illnesses, including chronic kidney disease, dementia, cardiovascular disease, diabetes, and ICU admission, may be viewed as risk factors for unfavourable results. In order to identify the factors that could accurately predict positive or negative outcomes, we characterised and analysed the clinical characteristics and prognoses of patients with Fusobacterium infections as well as underlying conditions.
Pathogenesis
Fusobacteria are part of the natural flora of the female vaginal tract, gastrointestinal tract, and oral cavity, and they are linked to both localised infections that are far away from these areas as well as contiguous, polymicrobial diseases.
Deoxyribonuclease, the development of a lipopolysaccharide capsule, neutrophil-cytotoxic factors, and other virulence factors have recently been identified in fusobacterial infections, despite the fact that the pathogenesis of these infections is still poorly understood.Infection is characterised by thrombosis, inflammation, and blood vessel invasion.
Both -lactamase, which defends organisms against -lactam antibiotics, and proteolytic enzymes, which facilitate invasion of local veins, are produced by fusobacteria.Fusobacterium may promote the growth of other anaerobic and aerobic organisms, according to research in animals.
Fusobacterial infections are most commonly caused by a propensity to invade through disturbance of the normal mucocutaneous barrier, which can happen in conditions like Epstein-Barr virus pharyngitis12 or mucositis brought on by chemotherapy and neutropenia. Low oxidation-reduction potential can be encouraged when microvascular illness affects the blood supply or tissue injury after an accident or surgical trauma, both of which can promote bacterial growth.
Physiological form and function of fusobacterium
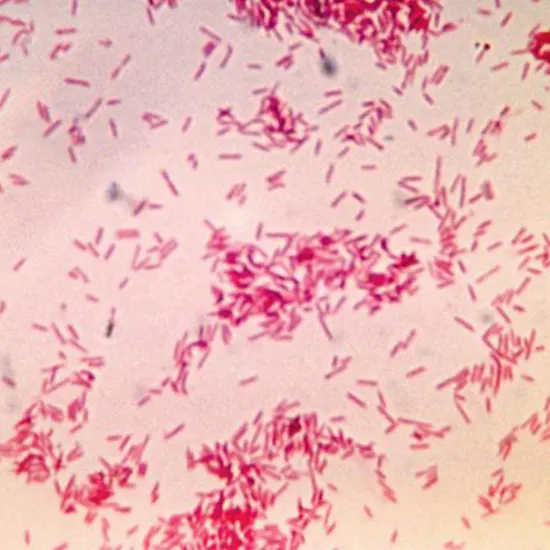
A mysterious subgroup of bacterial species is known as fusobacteria. These bacteria have piqued the interest of the scientific community for almost a century because they are difficult to grow, control, and comprehend. The Fusobacteria are now acknowledged as belonging to a phylum in their own right, despite first being categorised as an outgrowth of the Bacteroidaceae family based on their Gram-negative morphology, anaerobic lifestyle, and fermentative capabilities.
The Fusobacteria taxonomic cluster, as determined by 16S rRNA gene sequencing and comparison, is a very small phylum of the bacterial tree of life. It is made up of a single class, Fusobacteria, which includes a single order, Fusobacteriales, which branches into two families, Fusobacteriaceae and Leptotrichiaceae. One of the five recognised genera of the Fusobacteriaceae family, along with Cetobacterium, Ilyobacter, Propionigenium, and Psychrilyobacter, is Fusobacterium.
Since then, it has been discovered that Fusobacterium spp. share more characteristics with the Gram-positive Firmicutes than with other Gram-negative phyla, adding to the mystique surrounding this puzzling group.
The Fusobacteriaceae family proved challenging to classify using conventional morphological and biochemical tests before 16S rRNA gene sequences became often employed to separate bacterial taxa. For instance, the shape of fusobacterial colonies is heterogeneous and can vary even within members of the same species.
FUSOBACTERIUM INFECTIONS
Testing for susceptibility should always be done to help direct treatment. The majority of other obligate anaerobes and Fusobacterium species are resistant to ahminoglycosides. However, amino-glycosides are occasionally added for comprehensive coverage since infections with Fusobacterium are frequently combined with those caused by other non-anaerobic bacteria. For the purpose of removing necrotic tissue and promoting blood flow to the infection site, surgical drainage or debridement is crucial.
Methods for detection
From a computerised database, all cases of Fusobacterium spp. bacteraemia discovered at a local microbiology lab over the course of 11 years that provided outpatient and acute care for a population of C- Reactive Protein around 1.3 million people were identified. To identify underlying risk factors for and outcomes of infection, clinical data on these cases was retrieved from an administrative database and examined.
MANAGEMENT
Parenteral antibiotic administration is the main treatment for Lemierre disease. Treatment should include medicines that have efficacy against oral anaerobes that are resistant to beta-lactam antibiotics since some Fusobacterium species manufacture beta-lactamase enzymes. Ampicillin-sulbactam and clindamycin plus ceftriaxone with or without metronidazole are two options. For four to six weeks, intravenous therapy is continued. Monitoring for the spread of the septic thrombus or deteriorating pulmonary function requires vigilance.
Heparin anticoagulation is advised by some writers for Lemierre disease.Thrombophilia was confirmed in all 7 of the 9 Lemierre disease cases investigated in a sample of 9 cases that was published in 2005. Antiphospholipid antibodies and increased factor VIII activity primarily made up the prothrombotic condition. The median time spent on anticoagulation was three months.
All children have survived without experiencing recurrent venous thrombophlebitis after a median follow-up of one year. However, 38% of the children using anticoagulants continued to have vascular blockage of the internal jugular vein, which was diagnosed in the acute stage of the illness.
Metronidazole has a distinctive bactericidal effect on B. fragilis and C. perfringens as well as activity against stringent anaerobes, most B. fragilis strains, Fusobacterium spp., and Clostridium spp. Metronidazole resistance in B. fragilis is uncommon, despite the fact that 12.3% of B. fragilis isolates were found to be resistant in a South African survey.
Although there is some in vivo evidence in animal models and humans that metronidazole has activity against CT Scan Pelvis E. coli and other aerobes in mixed aerobic-anaerobic infections, the in vitro activity of metronidazole is poor against aerobes, microaerophiles, and anaerobes that may become aerotolerant on subculture. Despite the fact that the exact method is unknown.
However, because facultative gram-negative bacilli and microaerophilic gram-positive cocci (common copathogens in polymicrobial anaerobic infection) are resistant to metronidazole, the medication should be used in conjunction with another agent that is active against these pathogens to make up for these flaws in its spectrum.
The relative incidence of diarrhoea and colonisation caused by C. difficile was reported to be lower after using metronidazole than after Ultrasound clindamycin in a retrospective analysis. One of the preferred medications for treating this condition is metronidazole.
CONCLUSION
Infections with fusobacterium are infrequent. Younger people are more susceptible to infection from F. necrophorum than elderly patients are with F. nucleatum. The clinical spectrum is broad, ranging from localised, minor infections like sinusitis or pharyngitis to infections that can lead to abscesses and are life-threatening.
The culprit responsible for rare infections is a type of Fusobacterium. The general incidence that we discovered in our investigation is comparable with prior works. F. nucleatum prefers to infect elderly MRI Venography patients, but F. necrophorum typically infects younger people. The clinical spectrum is broad and includes anything from pharyngitis and sinusitis to septic shock and other upper respiratory tract infections.
Broad-spectrum antibiotics like metronidazole or carbapenems should be started as an empirical treatment until sample cultures Cervical Culture can produce any conclusive results. According to drug resistance and sensitivity, this treatment needs to be adjusted.









