The coughing up of blood or blood-stained mucus from the lungs, bronchi, larynx, or trachea is known as hemoptysis
When every breath counts- Hemoptysis:
The coughing up of blood or blood-stained mucus from the lungs, bronchi, larynx, or trachea is known as hemoptysis.
- To put it another way, the airway is bleeding.
- This can happen with lung cancer, certain cardiovascular disorders, and illnesses including pneumonia, bronchitis, or tuberculosis.
- At 300 mL, hemoptysis is regarded as enormous (11 imp fl oz; 10 US fl oz). There are often catastrophic injuries in situations like these. Choking poses more of a threat than bleeding does.
Blood or blood-tinged sputum is expelled from the lungs or tracheobronchial tree during hemoptysis.
How long ago was the disease identified?
- In ancient times, it was believed to be a supernatural or divine affliction and was often associated with tuberculosis, a disease that was prevalent in many parts of the world.
- The earliest known medical description of hemoptysis dates back to the 2nd millennium BCE in ancient Egypt, where it was recorded in the Ebers Papyrus. This document described hemoptysis as a symptom of tuberculosis and recommended the use of a range of herbal remedies, including juniper berries, to treat the condition.
- In ancient Greece, hemoptysis was also associated with tuberculosis and was described by Hippocrates, who recommended the use of wine and honey to treat the condition.
- In the 2nd century CE, the Greek physician Galen recognized hemoptysis as a sign of lung disease and recommended the use of opium and other remedies to alleviate the symptoms.
- During the Middle Ages, hemoptysis was often associated with bleeding disorders or pulmonary infections and was treated with a range of herbal remedies and bloodletting.
- In the 18th and 19th centuries, the development of modern medicine led to a better understanding of the underlying causes of hemoptysis and the development of more effective treatments.
- Today, hemoptysis is recognized as a symptom of a wide range of medical conditions, including tuberculosis, lung cancer, bronchitis, and pneumonia, among others.
Epidemiological facts about hemoptysis:
- According to research studies, the incidence of hemoptysis is estimated to be between 0.2% and 0.5% per year in the general population. The prevalence of hemoptysis is higher among smokers and individuals with a history of lung disease or chronic obstructive pulmonary disease (COPD).
- In terms of age, hemoptysis is more commonly seen in individuals over the age of 40. Men are also more likely to experience hemoptysis than women, although the reason for this difference is not fully understood.
- The mortality rate associated with hemoptysis varies depending on the underlying cause of the condition. For example, hemoptysis associated with lung cancer is associated with a higher mortality rate than hemoptysis associated with bronchitis or pneumonia. Prompt diagnosis and treatment are crucial in preventing complications and improving outcomes.
In conclusion, hemoptysis is a relatively rare but potentially serious symptom that can indicate a range of underlying medical conditions. Understanding the epidemiology of hemoptysis can help healthcare professionals identify individuals at increased risk of the condition and provide appropriate diagnosis and treatment.
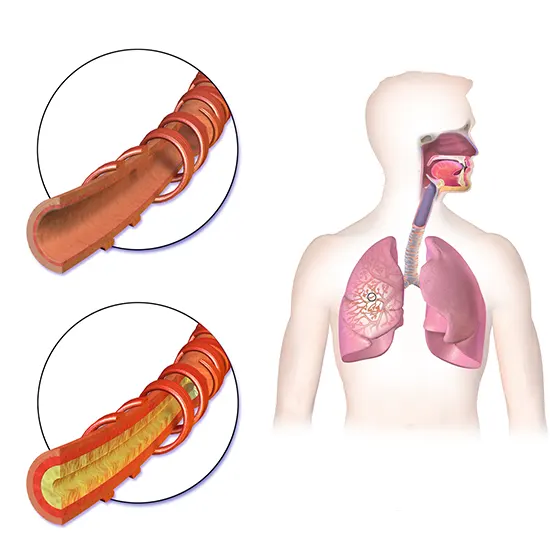
Pathophysiology of hemoptysis:
- Hemoptysis can be caused by a number of distinct pathologic pathways, depending on the underlying illness. The pulmonary and bronchial vessels are two distinct circulatory systems that are found in the lung. Either of these can result in hemoptysis.
- Many disorders can cause hemoptysis and infarction of the lung tissue. Hemoptysis is a common symptom of pulmonary emboli due to ischemic pulmonary parenchymal necrosis. All idiopathic vasculitis affecting the pulmonary arteries, including Wegener's granulomatosis, exhibit comparable ischemia necrosis. Staphylococcus aureus, Pseudomonas aeruginosa, Aspergillus fumigatus, and Phycomycetes are the most common infections that result in blood vessel invasion and infarction.
- Hemoptysis can also occur as a result of vascular engorgement and erosion. As a result of an acute infection like viral or bacterial bronchitis, a chronic infection like bronchiectasis, or a toxic exposure like cigarette smoke, this takes place within the bronchial capillaries.
- In frequent bacterial pneumonia such Streptococcus pneumonia, local hyperemia is present. Red hepatization of the lung, which occurs after vascular congestion, occurs when bacteria and blood-tinged fluid are added to neutrophils and fibrin in the alveoli of the lung. This causes the characteristically rust-colored, purulent sputum of pneumococcal pneumonia to be produced.
What are two types of hemoptysis?
There are two main types of hemoptysis:
- Massive hemoptysis
- Non-massive hemoptysis.
The distinction between these two types of hemoptysis is based on the volume of blood coughed up - massive hemoptysis is defined as the coughing up of more than 100 mL of blood within 24 hours.
- Massive Hemoptysis: Massive hemoptysis is a medical emergency and can be life-threatening. It is most commonly caused by bronchial artery rupture, which can be due to underlying lung cancer, tuberculosis, bronchiectasis, or other conditions that cause erosion of the blood vessels in the lungs. Massive hemoptysis can lead to hypovolemic shock, respiratory failure, and death if not treated promptly.
- Non-massive Hemoptysis: Non-massive hemoptysis is characterized by the coughing up of small amounts of blood or blood-tinged sputum. It is typically caused by less serious conditions, such as bronchitis, pneumonia, or inflammation of the airways due to allergies or irritants. While non-massive hemoptysis is generally less severe than massive hemoptysis, it can still be a cause for concern and should be evaluated by a healthcare professional to determine the underlying cause and appropriate treatment.
In addition to these two main types, hemoptysis can also be classified based on the source of bleeding within the respiratory tract.
For example, if the bleeding originates from the upper respiratory tract, it is referred to as epistaxis or nasal bleeding, while bleeding from the lower respiratory tract is classified as hemoptysis.
This distinction is important as it can help to identify the location and underlying cause of the bleeding, which can guide diagnosis and treatment.
What are the reasons for hemoptysis?
Here are some of the most common causes of hemoptysis:
- Lung infections: Hemoptysis can be a symptom of various respiratory infections, such as tuberculosis, bronchitis, pneumonia, and fungal infections.
- Lung cancer: Hemoptysis can be a sign of lung cancer, particularly when accompanied by other symptoms such as coughing, chest pain, and shortness of breath.
- Bronchiectasis: Bronchiectasis is a condition in which the airways in the lungs become damaged and widened, making them more susceptible to bleeding.
- Pulmonary embolism: Hemoptysis can be a symptom of a pulmonary embolism, which occurs when a blood clot blocks the blood vessels in the lungs.
- Chronic obstructive pulmonary disease (COPD): COPD, which includes chronic bronchitis and emphysema, can cause irritation and inflammation of the airways, leading to hemoptysis.
- Lung trauma: Hemoptysis can be caused by lung trauma, such as a puncture wound or injury from a car accident.
- Connective tissue disorders: Certain connective tissue disorders, such as Wegener's granulomatosis and Goodpasture's syndrome, can cause inflammation and damage to the blood vessels in the lungs, leading to hemoptysis.
- Blood disorders: Certain blood disorders, such as haemophilia and von Willebrand disease, can cause bleeding in the lungs and lead to hemoptysis.
- Drug use: Some drugs, such as cocaine, can cause irritation and damage to the airways and blood vessels in the lungs, leading to hemoptysis.
“Coughing up blood? Hemoptysis could be the cause”.
Other signs and symptoms includes:
Here are some of the common signs and symptoms of hemoptysis:
- Cough: Hemoptysis is often accompanied by a cough, which may be dry or productive.
- Blood in sputum: The most obvious symptom of hemoptysis is the presence of blood or blood-tinged sputum in the coughed-up material.
- Chest pain: Chest pain may occur if the hemoptysis is caused by lung infection, inflammation, or lung cancer.
- Shortness of breath: Shortness of breath or difficulty breathing may occur due to the loss of blood and the reduced oxygen-carrying capacity.
- Dizziness or lightheadedness: If there is significant blood loss, dizziness or lightheadedness may occur.
- Fever: Hemoptysis can be accompanied by a fever, especially if it is due to a lung infection.
- Rapid heartbeat: Rapid heartbeat or palpitations may occur in response to blood loss.
- Cyanosis: Cyanosis or bluish discoloration of the skin and mucous membranes may occur due to inadequate oxygenation of blood.
What should be the diagnostic approach for hemoptysis?
Here are some of the common diagnostic tests used to evaluate hemoptysis:
- Chest X-ray: A chest X-ray is usually the first test performed to evaluate hemoptysis. It can detect abnormalities in the lungs, such as tumours or infections.
- CT scan: A CT scan provides more detailed images of the lungs and can help identify small tumours or other abnormalities.
- Bronchoscopy: A bronchoscopy is a procedure in which a flexible tube with a camera is inserted through the mouth or nose into the airways to examine them for abnormalities or bleeding sources.
- Blood tests: Blood tests may be performed to evaluate blood clotting factors and other blood parameters.
- Arterial blood gas (ABG) analysis: ABG analysis can evaluate the oxygen and carbon dioxide levels in the blood.
- Sputum culture: Sputum culture can help identify the presence of infections or bacteria in the respiratory tract.
- Biopsy: In some cases, a tissue biopsy may be necessary to diagnose underlying conditions such as lung cancer.
“Early diagnosis is a key”
Don’t wait to get treatment
Treatment options include:
Here are some of the common treatment options for hemoptysis:
- Observation: If the hemoptysis is mild and resolves on its own, observation may be all that is needed.
- Medications: Depending on the underlying cause, medications such as antibiotics, corticosteroids, or anticoagulants may be prescribed.
- Bronchoscopy: If the bleeding source is identified during a bronchoscopy, interventions such as cauterization, laser therapy, or stenting may be performed to stop the bleeding.
- Surgery: In cases where the bleeding cannot be controlled by other methods or there is a suspected tumour or other structural abnormality, surgery may be necessary.
- Radiation therapy: Radiation therapy may be used to treat underlying lung cancer or other tumours causing hemoptysis.
- Pulmonary embolism treatment: Hemoptysis caused by pulmonary embolism may require immediate treatment with anticoagulants and other medications to dissolve the blood clot.
“Seek medical attention immediately”
What can be the differential diagnosis?
- Apart from the lower respiratory tract
- Greater airway (nasopharyngeal) bleeding.
- Bleeding from the gut.
- Source: tracheobronchial
- Bronchogenic carcinoma, endobronchial metastatic tumour, Kaposi's sarcoma, and bronchial carcinoid are examples of neoplasm.
- Bronchitis (acute or chronic)
- Bronchiectasis
- Broncholithiasis
- Airway injury
- Foreign object
Source of pulmonary parenchyma
- Lung infection
- Pneumonia
- Tuberculosis
- "Fungus ball," mycetoma
- The syndrome of Goodpasture
Hemoptysis vs others
In order to diagnose hemoptysis, your doctor will need to determine whether the blood is coming from your lungs, upper respiratory tract, upper digestive tract, or both.
It's known as pseudo hemoptysis. Alternatively, you can be experiencing hematemesis, which is the vomiting of blood.
- Sputum (the substance you cough up), which is caused by hemoptysis, is bright red or pink and foamy.
- Pseudohemoptysis resembles it extremely closely. Tests may be the only way to distinguish between the two.
- The substance that hematemesis produces is darker and resembles coffee grinds. It might be combined with food scraps.
Prognosis of hemoptysis:
A prognosis for hemoptysis depends on the underlying cause and the severity of the condition. Some causes, such as a minor respiratory infection, may resolve on their own with rest and home remedies. Other causes, such as lung cancer, can be serious and require prompt medical attention.
The prognosis and treatment plan for hemoptysis will depend on the cause and severity of the condition and may include medication, surgery, or other interventions as necessary. It's important to follow your doctor's instructions and attend all follow-up appointments to manage the condition effectively.
What if left untreated?
Some potential complications of hemoptysis include:
- Anaemia: Hemoptysis can lead to a significant loss of blood, which can cause anaemia, a condition where the body doesn't have enough healthy red blood cells to carry oxygen to the body's tissues.
- Respiratory distress: In severe cases of hemoptysis, the patient may experience difficulty breathing or respiratory distress, which can lead to low oxygen levels in the body.
- Aspiration: Coughing up blood can increase the risk of aspiration, where blood or other materials enter the lungs, potentially causing infection or other complications.
- Shock: Severe cases of hemoptysis can lead to a dangerous drop in blood pressure and may result in shock, a life-threatening condition that requires immediate medical attention.
- Infection: Hemoptysis can increase the risk of developing lung infections, which can further complicate the underlying condition and require additional treatment.
- Emotional distress: Hemoptysis can be a frightening and distressing symptom for patients, and it can lead to anxiety, depression, and other emotional and psychological issues.