Hypoxia is a condition in which the body's tissues do not have access to enough oxygen to maintain healthy homeostasis. Insufficient blood flow to the tissues is the main reason. Acute, chronic, or acute and chronic...
Hypoxia : When you can’t breathe every moment matters
Hypoxia is a condition in which the body's tissues do not have access to enough oxygen to maintain healthy homeostasis. Insufficient blood flow to the tissues is the main reason.
Acute, chronic, or acute and chronic types of hypoxia can manifest and range in severity from moderate to severe.
Hypoxia has different effects on different tissues. While some tissues can withstand certain types of hypoxia or ischemia for a longer period of time, other tissues are severely harmed by low oxygen levels.
Cyanosis : Blue is not just a colour, it's a warning sign.
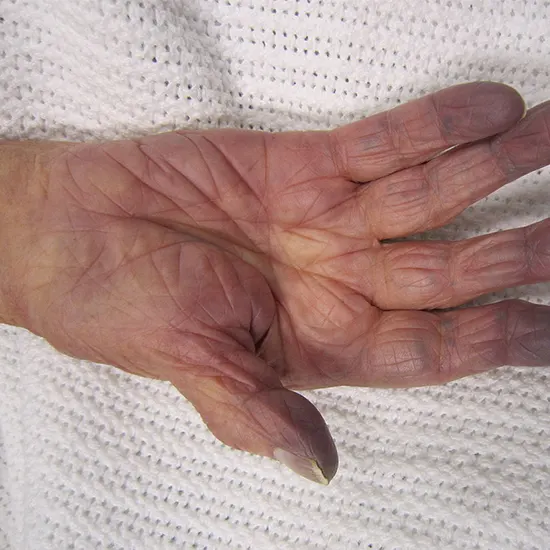
A bluish staining of the skin or mucous membranes is a pathologic condition known as cyanosis.
Cyan, a blue-green colour, is the root of the word cyanosis.
Cyanosis can present a significant diagnostic problem.
The cause can be determined with the aid of a thorough evaluation and the appropriate diagnostic equipment.
What can be the pathogenesis?
Hypoxia
The process of hypoxia pathogenesis involves a cascade of events, including the following:
Decreased oxygen supply : This is the primary cause of hypoxia, and it can be due to a variety of factors, including low oxygen in the air, lung diseases that impair breathing, reduced oxygen-carrying capacity of the blood, and reduced blood flow to tissues.
Reduced oxygen diffusion : Oxygen moves from areas of high concentration to low concentration. In hypoxia, there is a reduced concentration of oxygen in the tissues, which reduces the rate of oxygen diffusion into the tissues.
Cellular hypoxia : Reduced oxygen supply and diffusion lead to cellular hypoxia, which is the insufficient oxygen supply to the body's cells. Cellular hypoxia can cause damage to cell structures, impair cellular function, and lead to cell death.
Anaerobic metabolism : When there is a lack of oxygen, cells switch to anaerobic metabolism, which produces less energy and more waste products. This can further impair cellular function and lead to tissue damage.
Ischemia : If hypoxia persists, it can lead to ischemia, which is the death of tissues due to a lack of oxygen supply.
In summary, the pathogenesis of hypoxia involves a complex interplay of factors that lead to a reduced oxygen supply, cellular hypoxia, anaerobic metabolism, and tissue damage. Prompt recognition and treatment of hypoxia is essential to prevent further complications and tissue damage.
Cyanosis
The process of cyanosis pathogenesis involves the following:
Reduced oxygen supply : This is the primary cause of the cyanosis, and it can be due to a variety of factors, including lung diseases that impair breathing, heart diseases that reduce blood flow to the lungs, and reduced oxygen-carrying capacity of the blood.
Deoxygenation of haemoglobin : When there is a reduced oxygen supply, the haemoglobin in the blood binds with less oxygen, resulting in the formation of deoxygenated haemoglobin.
Blood shunting : In some cases, blood may bypass the lungs and go directly to the systemic circulation, leading to reduced oxygenation of the blood.
Increased extraction of oxygen by tissues : When there is reduced oxygen delivery to the tissues, the tissues may increase their extraction of oxygen, resulting in a greater proportion of deoxygenated haemoglobin in the blood.
Cyanosis : The presence of deoxygenated haemoglobin in the blood gives it a bluish tint, which can be seen in the skin and mucous membranes.
Tissue hypoxia : If cyanosis persists, it can lead to tissue hypoxia, which is the insufficient oxygen supply to the body's cells. Tissue hypoxia can cause damage to cell structures, impair cellular function, and lead to cell death.
In summary, the pathogenesis of cyanosis involves a complex interplay of factors that disrupt the normal oxygenation of the blood, leading to the presence of deoxygenated haemoglobin in the blood and bluish discoloration of the skin and mucous membranes. Prompt recognition and treatment of the underlying cause of cyanosis are essential to prevent further complications and tissue damage.
What are the types of these conditions?
Cyanosis
There are several types of cyanosis, including
- Central cyanosis: This type of cyanosis is caused by a decrease in the amount of oxygen in the arterial blood, which results in the blue discoloration of the lips, tongue, and nail beds. Central cyanosis is usually a sign of a serious underlying medical condition, such as heart or lung disease.
- Peripheral cyanosis: This type of cyanosis is caused by reduced blood flow to the extremities, such as the fingers and toes, resulting in a bluish coloration of the skin. Peripheral cyanosis can be caused by cold temperatures, peripheral vascular disease, or Raynaud's phenomenon.
- Acrocyanosis: This is a type of peripheral cyanosis that is characterised by a blue or purple discoloration of the hands and feet, which occurs due to the constriction of small blood vessels in the skin.
- Methemoglobinemia: This is a rare condition in which there is an abnormal form of haemoglobin in the blood, which cannot bind oxygen effectively. Methemoglobinemia can cause cyanosis and can be caused by certain medications or genetic factors.
- Hypoxemia: This is a general term for low levels of oxygen in the blood, which can lead to central cyanosis. Hypoxemia can be caused by a variety of medical conditions, such as pneumonia, asthma, or heart failure.
Hypoxia:
Here are some of the common types of hypoxia
Hypoxic hypoxia: This type of hypoxia occurs when there is a decrease in the amount of oxygen in the air we breathe. For example, high altitude areas where the air pressure is low can cause hypoxic hypoxia.
Anaemic hypoxia: This type of hypoxia occurs when there is a decrease in the amount of oxygen-carrying capacity of the blood due to anaemia or other blood disorders.
Circulatory hypoxia: This type of hypoxia occurs when there is inadequate blood circulation to the body tissues, preventing oxygen from reaching the cells. Causes include heart failure, shock, and blood vessel obstruction.
Histotoxic hypoxia: This type of hypoxia occurs when the cells are unable to use the oxygen in the blood effectively. Causes include alcohol and drug poisoning.
Hemic hypoxia: This type of hypoxia occurs when there is a reduction in the amount of haemoglobin available to carry oxygen in the blood, such as in carbon monoxide poisoning.
What is the similarity between hypoxia and cyanosis?
Similarities between hypoxia and cyanosis:
- Both hypoxia and cyanosis are caused by insufficient oxygen delivery to the body's tissues.
- Hypoxia and cyanosis can both be signs of an underlying medical condition, such as lung disease, heart failure, or anaemia.
- Both hypoxia and cyanosis can result in shortness of breath, dizziness, and confusion.
- Hypoxia can cause cyanosis, as low oxygen levels in the blood can lead to a bluish discoloration of the skin and mucous membranes.
- Cyanosis can indicate the presence of hypoxia, as it is a visible sign that the body is not receiving enough oxygen.
- Both hypoxia and cyanosis require prompt medical attention, as they can be life-threatening if left untreated.
What are the common causes of hypoxia and cyanosis?
Here are some common causes of hypoxia and cyanosis
Lung diseases such as chronic obstructive pulmonary disease (COPD), asthma, and pneumonia can cause hypoxia and cyanosis.
Heart diseases such as congestive heart failure, coronary artery disease, and heart defects can cause hypoxia and cyanosis.
Anaemia, which is a deficiency of red blood cells or haemoglobin in the blood, can cause hypoxia and cyanosis.
High altitudes, where the air pressure and oxygen levels are lower, can cause hypoxia and cyanosis.
Carbon monoxide poisoning, which can occur from exposure to smoke or fumes, can cause hypoxia and cyanosis.
Shock, which is a medical emergency characterised by low blood pressure and decreased blood flow, can cause hypoxia and cyanosis.
Hypothermia, which is a drop in body temperature, can cause peripheral cyanosis due to decreased blood flow to the extremities.
Certain medications, such as opioids and sedatives, can cause respiratory depression and hypoxia.
To summarise this, hypoxia and cyanosis can have various causes, ranging from respiratory and cardiovascular diseases to environmental factors and medication use. Prompt medical attention is necessary to determine the underlying cause and provide appropriate treatment.
Don't suffer in silence- tell your doctor if you feel any of these symptoms.
Here are some common signs and symptoms of hypoxia and cyanosis:
- Shortness of breath or difficulty breathing.
- Rapid or shallow breathing.
- Wheezing or chest tightness.
- Fatigue or weakness.
- Confusion or disorientation.
- Headache or lightheadedness.
- Blue discoloration of the skin, lips, or fingernails (cyanosis).
- Fast heart rate or palpitations.
- Sweating or clammy skin.
- Dizziness or fainting.
- Cyanosis in the mucous membranes, such as in the mouth or tongue.
- Decreased cognitive function or memory impairment.
- Blurred vision or visual disturbances.
- Nausea or vomiting.
- Seizures or convulsions.
When in doubt, Check it out
Diagnosis of hypoxia and cyanosis:
Here are some common diagnostic tools used for hypoxia and cyanosis:
Pulse oximetry : This is a non-invasive test that measures the oxygen saturation in the blood using a device attached to the finger or earlobe.
Arterial blood gas (ABG) analysis : This test involves taking a sample of arterial blood to measure the oxygen and carbon dioxide levels and determine the pH of the blood.
Chest X-ray : This test (Chest X-Ray) is used to evaluate the lungs and determine if there is any underlying lung disease or injury.
Electrocardiogram (ECG) : This test (Electrocardiogram) is used to evaluate the heart's electrical activity and detect any abnormalities that may be causing hypoxia and cyanosis.
Echocardiogram : This test uses ultrasound waves to evaluate the heart's structure and function and can identify any abnormalities that may be causing hypoxia and cyanosis.
Pulmonary function tests : These tests (PFT) measure the lung's ability to take in and release air and can identify any underlying lung disease.
Blood tests : These tests can evaluate the levels of red blood cells and haemoglobin in the blood, which can help diagnose anaemia as a cause of hypoxia and cyanosis.
What can be the treatment options as every breath counts
Here are some common treatment options:
Oxygen therapy: This is the primary treatment for hypoxia and involves providing supplemental oxygen to increase oxygen levels in the blood. Oxygen can be delivered through a nasal cannula, face mask, or other devices.
Medications: Depending on the underlying cause of hypoxia and cyanosis, medications may be prescribed to treat lung or heart disease, anaemia, or other conditions.
Mechanical ventilation: In severe cases of hypoxia, mechanical ventilation may be necessary to help the patient breathe and improve oxygen levels.
Surgery: In cases where heart or lung disease is causing hypoxia and cyanosis, surgery may be necessary to repair or replace damaged tissues or organs.
Lifestyle modifications : Making lifestyle changes such as quitting smoking, maintaining a healthy weight, and exercising regularly can help improve lung function and prevent or manage hypoxia and cyanosis.
Treating underlying medical conditions : Hypoxia and cyanosis can be caused by a variety of medical conditions, so treating the underlying condition is essential in managing the symptoms.
What can be the prognosis for both disorders?
The prognosis for hypoxia and cyanosis depends on the underlying cause, the severity of the condition, and the promptness and effectiveness of treatment. In some cases, hypoxia and cyanosis can be mild and resolve on their own, while in other cases, they can be severe and life-threatening.
If left untreated or inadequately treated, hypoxia and cyanosis can lead to serious complications, such as respiratory failure, heart failure, or organ damage, and can be fatal. Prompt treatment can improve outcomes and prevent complications.
The prognosis also depends on the individual's overall health and the presence of any other medical conditions. Individuals with underlying lung or heart disease, anaemia, or other medical conditions may have a more guarded prognosis.
It is essential to seek medical attention promptly if you experience symptoms of hypoxia and cyanosis, such as shortness of breath, rapid breathing, or blue discoloration of the skin or mucous membranes.
What can be the possible complications if left untreated?
Some common complications associated with hypoxia and cyanosis:
Organ damage : When the body's tissues and organs are deprived of oxygen, they can sustain damage, especially the brain, heart, and lungs.
Respiratory failure : Hypoxia can lead to respiratory failure, a condition in which the body's respiratory system cannot provide enough oxygen to maintain normal bodily functions.
Cardiac arrest : In severe cases of hypoxia and cyanosis, the heart can stop beating, leading to cardiac arrest, which is a medical emergency.
Developmental delays : Prolonged hypoxia in infants and children can lead to developmental delays and neurological damage.
Pulmonary hypertension : Hypoxia can cause pulmonary hypertension, a condition in which the blood vessels in the lungs constrict and increase the pressure in the lungs, leading to heart failure.
Cognitive impairment : Prolonged hypoxia can cause cognitive impairment, including memory loss, confusion, and difficulty concentrating.
Organ failure : In severe cases, hypoxia and cyanosis can lead to multi-organ failure, which is a life-threatening condition that requires immediate medical attention.









