Kingella kingae was believed to be a rare bacteria up to the most recent development in diagnostic methods. In children between the ages of 6 and 48 months, kingella kingae is now recognised as a prominent cause of paediatric...
Kingella kingae was believed to be a rare bacteria up to the most recent development in diagnostic methods. In children between the ages of 6 and 48 months, kingella kingae is now recognised as a prominent cause of paediatric bacteraemia and bone infections. It is one of the possible causes of disease outbreaks in daycare centres in the US and other nations.
Kingella kingae is naturally present in the oropharyngeal lining of infants between the ages of 6 and 48 months, but it can enter the circulation through damaged mucosa and cause systemic infections. K. kingae infections often have modest symptoms, with the exception of endocarditis and osteoarticular infections.
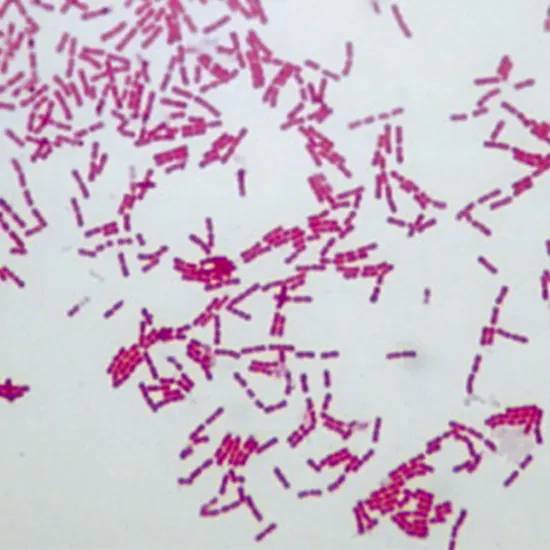
Etiology
Fastidious, gram-negative, facultative anaerobic coccobacillus belonging to the Neisseriaceae family is K. kingae. It is a beta-hemolytic bacterium that causes a ring of sporadic hemolysis. It is not mobile and does not produce spores. Although all strains have significant oxidase activity, catalase, indole, and urease do not cause any reactions in them.Blood agar, chocolate agar, and GC-based media all support the growth of K. kingae, while MacConkey or Krigler agar do not. K. kingae can have spreading or non-spreading growth patterns, both with fringes, or it can have dome-shaped growth patterns without any fringe.
Epidemiology
Although it is still unclear how widespread the illness is, invasive K. kingae is becoming more common in Israel, Western Europe, and the United States. Children, especially those under four years old, are most commonly affected by the bacterial infection known as Kingella kingae. Compared to colonisation rates of less than 1% for the age group of 0 to 6 months and in adults, K. kingae colonisation rates in children aged 1 to 4 years old range from 10 to 28%. It is thought that men are more likely than women to experience it. A significant incidence of invasive Kingella kingae infection is linked to social factors like nursery attendance.
Pathophysiology
For effective colonisation, carriage, transmission, virulence, and pathogenesis, K. kingae expresses many structures. Direct contact between people is how K. kingae is spread. Even if the exact mode of communication is unknown, droplets have a significant chance of being the means of transmission. Rho 54, pilS, and pilR genes control how K. kingae makes type IV pili (T4P).The Ultrasound Whole Abdomen respiratory mucosa and synovial membranes' sticky protein extensions are called pili. Virtually usually, a previous or concurrent viral illness is linked to bacterial invasion of the respiratory mucosa[8]. The herpangina virus, which causes hand, foot, and mouth disease, the herpes simplex virus, and human rhinovirus are frequently mentioned as commonly implicated viruses.
In addition to the RTA toxin produced by the bacterium, invasive K. kingae infection develops itself through a prior virus-induced mucosal injury. Leukocytes, macrophages, and synovial cells are all cytotoxic when exposed to RTA toxin. The outer-membrane's polysaccharide capsules provide defence CECT Chest against bacterial cells being phagocytes. The propensity of K. kingae to form biofilms aids the pathogen in subverting host defences and immunity. Exopolysaccharides of K. kingae also enable the periodic release of the bacterium cells from biofilms and have inhibitory effects on the creation of biofilms from other microorganisms, making it simpler to spread the bacteria.
Symptoms
Most infections affect young, healthy children under four or older children and adults who have impaired immune systems.
With the exception of quickly advancing endocarditis, where high fever, back pain, and night sweats are frequently reported, K. kingae symptoms are typically modest, with or without a slight temperature. Upper respiratory tract symptoms in the past or present or diarrhoea are common and may hint at an early suspicion.
Infection of the skeletal system
For children under the age of four, K. kingae is the most common cause of skeletal system infection. Due to the less severe inflammatory response brought on by the bacteria than other typical organisms causing osteoarticular infections, the symptoms may be subtly shown and patients typically arrive during the second week of infection.
Infected arthritis
The most prevalent type of osteoarticular disease found in K. kingae is this ailment. The knee is frequently implicated as the illness most frequently impacts the lower extremity. It's possible that more than one joint will be affected. The typical signs and symptoms of septic arthritis, such as localised pain, swelling, warmth, erythema, immobility, or joint effusion, may be present in patients. There can be less obvious fever.
Osteomyelitis
Long bones in the lower extremity are more commonly affected and are most frequently present in a subacute state. The involvement of bones including the clavicle, sternum, and calcaneus highlights K. kingae's relationship with unusual places.
Spondylodiscitis
It is difficult to walk or sit due to spondylodiscitis, an infection of the intervertebral disc space and surrounding vertebrae. In addition, children who have aberrant gait and back pain or stiffness. The afflicted intervertebral disc is usually one in the lumbar area, which is most typically affected. Intervertebral and spinal subdural abscess formation may also be related to K. kingae spondylodiscitis.
Bacteremia
Without any localised infection (occult bacteremia), or concurrently with other invasive infections, K. kingae can be isolated from the blood. The second most typical paediatric patient presentation is occult bacteremia.Without any signs of bone or joint infections, some people may have skeletal system concerns. X-Ray Acute infections such upper respiratory or gastrointestinal tract infections often cause concomitant symptoms in youngsters. A diffused maculopapular rash resembling that of meningococcal or gonococcal infections is uncommon in patients with occult bacteremia.In the event of a fever, it is often mild.
Infected soft tissues
Kingella kingae can cause abscesses in various places as well as a variety of soft tissue diseases such cellulitis, bursitis, tenosynovitis, and dactylitis.
Evaluation
The organisms can be found using both microbiological culture and nucleic acid amplification techniques. Although with erratic results, the organism can grow on blood culture vials (BCV) and other solid media like blood agar. Blood, lung cultures, and specimens from the skeletal system can all be used to culture bacteria. Today, advanced nations utilise the nucleic acid amplification assays. Compared to blood cultures, it is quicker and more sensitive.
Complete blood counts CBC , C- reactive protein (CRP) values, and radiographic tests should all be included in additional workups as necessary.
All children with invasive illness should get a transthoracic echocardiography to rule out endocarditis.
Treatment
As part of the conventional approach for treating serious bacterial infections, intravenous broad-spectrum second- or third-generation cephalosporins or penicillinase-stable beta-lactam antibiotics should be used as initial empiric therapy while waiting for culture results. Once K. kingae has been identified, the treatment plan should be switched to parenteral ampicillin if beta-lactamase-producing strains are absent or ampicillin/sulbactam if they exist. There are also other cephalosporins like cefuroxime and ceftriaxone that can be used.
Septic arthritis: The current standard is two to three weeks of intravenous-oral antibiotics taken in succession.
Osteomyelitis : The typical course of treatment is 3–6 weeks.
Traditional antibiotic therapy for spondylodiscitis lasts 3 to 12 weeks.
Prognosis
If identified and treated in a timely manner, the majority of invasive Kingella kingae infections are benign. The majority of Kingella kingae strains, with the exception of those that are beta-lactamase resistant, are sensitive to the majority of paediatric antibiotics. Osteoarticular infections in children frequently result in full recovery without any problems. Kingella spondylodiscitis can cause intravertebral abscess, however it is treatable with antibiotics. It is uncommon for complications to cause intervertebral discs to narrow.