Chronic infectious disorders that affect the skin and underlying tissues include actinomycetoma and eumycetoma. While eumycetoma is brought on by certain species of fungi, actinomycetoma is brought on by a group of bacteria...
Chronic infectious disorders that affect the skin and underlying tissues include actinomycetoma and eumycetoma. While eumycetoma is brought on by certain species of fungi, actinomycetoma is brought on by a group of bacteria known as Actinomycetes.
Actinomycetoma frequently manifests as a slowly growing mass or nodule that has the potential to bleed and exude pus. Actinomycetoma-causing bacteria are typically soil-dwelling organisms Histoplasma Antibody immunodiffusion that enter the body through a skin incision or abrasion. Actinomadura madurae, Streptomyces , and Nocardia are the most prevalent Actinomycetes species that result in actinomycetoma.
of Actinomycetoma and Eumycetoma:
The conditions actinomycetoma and eumycetoma are not universal, hence they are not seen everywhere.
In rural areas where people work barefoot or with inadequate footwear, exposing their feet to soil and other environmental toxins, these situations are more prevalent in tropical and subtropical countries.
There are several regions of the world where actinomycetoma and eumycetoma are more common, including Latin America, Africa, and Asia.
These illnesses are regarded as endemic in several nations, such Sudan and Mexico, where they often occur and have a substantial impact on the populace.
Causes and Risk factor for the infection of Actinomycetoma and Eumycetoma:
The bacteria (Actinomycetoma) or fungi (Eumycetoma) that cause these diseases enter the body through cuts or wounds. The following are some of the root causes and risk factors for these infections:
Actinomycetoma and eumycetoma causes:
Bacteria from the Actinomycetaceae family, including Actinomadura, Nocardia, and Streptomyces, are the culprits behind actinomycetoma.
Fungi like Madurella mycetomatis, Madurella , and Exophiala are responsible for eumycetoma.
Actinomycetoma and Eumycetoma risk factors include:
The risk of contracting these illnesses increases when people live in unsanitary and unhygienic environments.
Due to their regular exposure to soil and water, farmers, herders, and other outdoor workers are more at risk.
Skin trauma, such as a cut or puncture wound, can give bacteria or fungi a point of entrance.
The risk of contracting these infections can be increased by uncontrolled diabetes and other immune-depressing disorders.
Long-term use of some drugs, like corticosteroids, can raise the chance of contracting these illnesses.
Signs and Symptoms of Actinomycetoma and Eumycetoma:
Actinomycetoma
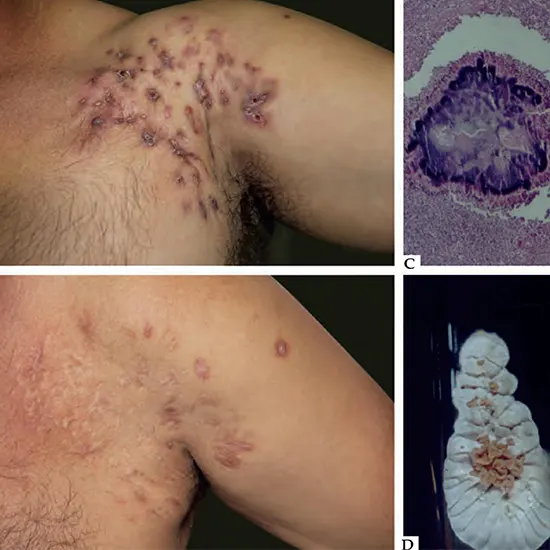
Although it can occur in other parts of the body, actinomycetoma is a persistent bacterial infection that primarily affects the skin and soft tissues of the feet and legs. Actinomycetoma commonly manifests as some of the symptoms and warning indications listed below:
- Pain and swelling: The affected area may seem uncomfortable and swollen.
- Ulcers: The skin may get infected with open sores or ulcers that are difficult to heal.
- Pus or other discharge may be present in the affected area.
- Hard nodules or lumps may grow beneath the skin as a result of the infection.
- Destruction of soft tissue and bone that, if left untreated, could result in deformity or handicap
- In rare situations, advanced cases may show systemic signs as fever, lethargy, and weight loss.
Eumycetoma:
Subcutaneous nodules that grow slowly and without pain over months to years, frequently on the foot or hand.
Lesions that may turn from pink to brown or black and have a stiff, rubbery, or woody texture.
pus-, blood-, or black granule-draining sinuses or fistulas (sometimes known as "fungal grains".
Heat, redness, and localised swelling surrounding the lesion.
Destructive bone and soft tissue alterations that, if addressed, can result in disability or amputation.
It is unusual to experience systemic symptoms including fever, exhaustion, and weight loss.
Diagnosis of Actinomycetoma and Eumycetoma:
Imaging investigations, laboratory tests, and clinical examinations can all be used to diagnose actinomycetoma and eumycetoma. The following are some typical techniques for detecting these ailments:
Actinomycetoma:
Physically examining the lesion may reveal subcutaneous nodules, sinuses or fistulas that drain, as well as granules or pus.
Microscopic analysis of the biopsy sample or draining material, which may reveal sulphur granules and gram-positive branching filaments known as actinomycetes.
The ability to confirm the presence of actinomycetes and determine the species involved through culture of the draining material or biopsy specimen.
Imaging tests like X-rays, CT scans, or MRIs can detect changes in the soft tissues and bones and can assist diagnose the severity of an infection.
Eumycetoma:
When the lesion is physically examined, subcutaneous nodules, sinuses or fistulas that are draining, fungal grains, or pus may all be seen.
Microscopic analysis of the biopsy sample or draining material, which may reveal fungus hyphae and spores.
It is possible to establish the presence of fungus and determine the species involved by the culture of the draining material or a biopsy specimen.
Serologic testing, which could find particular antibodies in the patient's blood against the harmful fungi.
Imaging tests like X-rays, CT scans, or MRIs can reveal changes in the bones and soft tissues and help doctors estimate the severity of the illness.
It is significant to highlight that actinomycetoma and eumycetoma diagnosis can be difficult and necessitates specialised laboratory knowledge. It is best to get the advice of a qualified healthcare practitioner to confirm the diagnosis and determine the most suitable course of action.
Various Treatment options for Actinomycetoma and Eumycetoma Infection
Chronic infections that affect the skin, subcutaneous tissues, and scan bones include actinomycetoma and eumycetoma. Eumycetoma is caused by fungi, but actinomycetoma is caused by bacteria. These infections are hard to treat and need ongoing treatment. The following are some options for treating actinomycetoma and eumycetoma:
Antimicrobial therapy with a mix of antibiotics is the first line treatment for actinomycetoma. Tetracyclines, aminoglycosides, and sulfonamides are the most often prescribed antibiotics. Typically, a course of treatment lasts six months to a year.Antifungal therapy is used to treat eumycetoma, and the choice of antifungal medication is determined by the fungus that is the cause. Itraconazole and ketoconazole are the two antifungal drugs that are most frequently utilised.
Actinomycetoma and eumycetoma can both be effectively treated with surgical excision. It frequently works in conjunction with antifungal or antibacterial therapy. Surgery aims to remove as much contaminated tissue as possible in order to increase the effectiveness of antibiotic or fungal treatment.
Amputation: In some circumstances, an amputation may be required to entirely remove the affected tissue. When other therapies have failed or the infection has reached the bone, this is frequently the case.
Actinomycetoma and eumycetoma have both been treated with adjunctive hyperbaric oxygen therapy (HBOT). 100% oxygen is inhaled in a high-pressure chamber, which can increase oxygen transport to sick tissues and boost the effectiveness of antibiotics and antifungal medications.
Immunotherapy : In cases of actinomycetoma, immunotherapy with a vaccination against the causing agent has been explored with varying degrees of success.
Actinomycetoma and eumycetoma treatment can be difficult and necessitates a team effort between surgeons, infectious disease experts, and other medical personnel. The severity of the infection, the agent responsible for it, and the patient's general state of health all influence the treatment option.
Prevention and Prognosis of Eumycetoma and Actinomycetoma:
Prevention:
Avoiding exposure to the factors that cause actinomycetoma and eumycetoma is the best strategy to prevent them.
These infections are more likely to affect people who work in agriculture, forestry, and construction.
They should take preventative measures to avoid suffering skin injuries, such as using protective clothing and footwear and staying away from polluted surfaces like soil and water. Additionally, good hygiene habits like routine foot and hand washing might aid in preventing these ill.
Prognosis
The prognosis of actinomycetoma and eumycetoma is influenced by a number of variables, such as the severity of the infection, the agent that caused it, and how well the patient responds to treatment. Even with therapy, Gram Stain these infections can persist for years. The prognosis improves with earlier diagnosis and therapy.
The prognosis of actinomycetoma is often better than that of eumycetoma. Antimicrobial therapy and surgical excision are effective treatments for actinomycetoma.
The cure rate can reach 80% with early treatment. Eumycetoma, on the other hand, has a lower cure rate and is more challenging to treat. Depending on the fungus that is causing the infection, different antifungal treatments work differently, and surgery is frequently needed to entirely remove the affected tissue. The cure rate for eumycetoma is only between 30 and 50%, even with treatment.
Recurrence is a possibility with both types of infections, particularly if the course of therapy is not followed if the root cause is not entirely eliminated. Monitoring for problems and recurrence over an extended period of time is essential.
In conclusion, long-term treatment is necessary for the chronic infections actinomycetoma and eumycetoma. Antimicrobial therapy, surgical excision, and hyperbaric oxygen therapy are all available as treatments. Avoiding exposure to the harmful substances and maintaining proper hygiene are key components of prevention.
Better outcomes can be achieved with early diagnosis and treatment, and ongoing research is required to enhance the lives of those who are afflicted.








.webp)