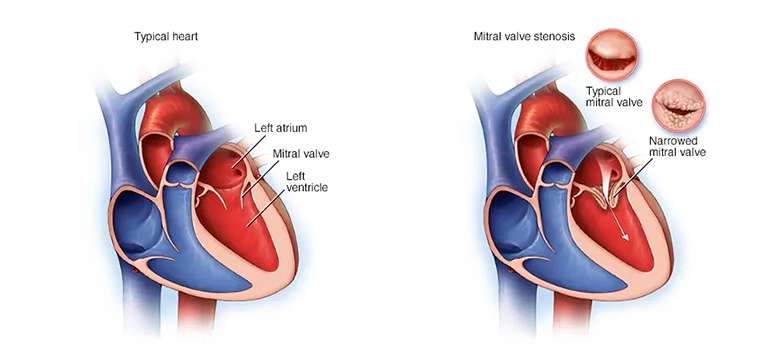
Mitral Stenosis (MS) is a heart condition characterized by the narrowing of the mitral valve, which separates the left atrium and the left ventricle. It is a form of valvular heart disease that can impact the heart's...
Mitral Stenosis (MS) is a heart condition characterized by the narrowing of the mitral valve, which separates the left atrium and the left ventricle. It is a form of valvular heart disease that can impact the heart's ability to pump blood efficiently.
In this article, we will explore the causes, symptoms, diagnosis, and treatment options for Mitral Stenosis, shedding light on this significant cardiac condition.
Table of Contents:
- What is Mitral Stenosis?
- Causes and Risk Factors
- Signs and Symptoms of Mitral Stenosis
- Treatment for Mitral Stenosis
- Conclusion
What is Mitral Stenosis
Understanding Mitral Stenosis (MS) starts with recognizing its impact on the heart's function. It's a heart condition where the mitral valve, separating the left atrium and ventricle, becomes narrow. This narrowing restricts blood flow, causing increased pressure in the left atrium and potential fluid accumulation in the lungs.
Causes and Risk Factors of Mitral Stenosis
Mitral Stenosis (MS) can have various causes and risk factors that contribute to its development. Understanding these factors is essential for early detection and effective management.
By understanding the anatomy and physiology of MS, we can grasp the importance of early detection and effective management for optimal heart function and overall well-being.
Let's explore the causes and risk factors of MS in detail:
Rheumatic Fever: The most common cause of Mitral Stenosis is rheumatic fever. This inflammatory condition occurs as a complication of untreated streptococcal throat or scarlet fever infections. Over time, the inflammation affects the mitral valve, leading to its narrowing and the subsequent development of MS.
Congenital Heart Defects: Some individuals are born with structural abnormalities in the mitral valve, which can contribute to the development of MS later in life. These defects can include a smaller valve size or abnormal valve leaflets, impairing proper blood flow through the valve.
Autoimmune Conditions: Certain autoimmune disorders, such as systemic lupus erythematosus or rheumatoid arthritis, can increase the risk of developing Mitral Stenosis. The immune system's abnormal response may cause inflammation and damage to the mitral valve, resulting in its narrowing.
Aging: With age, the mitral valve may naturally degenerate and become calcified, a condition known as mitral valve sclerosis. This calcification can progressively lead to Stenosis and the development of MS.
Earlier Mitral Valve Infections: Individuals who have had previous infections or endocarditis affecting the mitral valve are at an increased risk of developing MS. The infection can cause scarring and damage to the valve, leading to its narrowing over time.
Women are more prone: Women are more commonly affected by Mitral Stenosis compared to men. The reasons behind this gender disparity are not entirely understood, but hormonal and genetic factors may play a role.
Topography: In some regions, particularly those with a high prevalence of rheumatic fever, the incidence of Mitral Stenosis is higher. This highlights the impact of geographical factors and healthcare access on the development of this condition.
Genetics: There may be a genetic predisposition to developing Mitral Stenosis. If individuals have a family history of MS or other heart valve disorders, their risk of developing the condition may be increased.
By recognizing these causes and risk factors of Mitral Stenosis, individuals and healthcare professionals can be more vigilant in monitoring the condition, implementing preventive measures, and ensuring timely interventions. Early detection and appropriate management are crucial to minimizing the impact of MS and improving overall heart health.
Signs & Symptoms of Mitral Stenosis
Following are the signs and symptoms of Mitral Stenosis:
Fatigue and Weakness: Individuals with Mitral Stenosis may experience persistent fatigue and a general feeling of weakness, even with minimal physical exertion.
Shortness of Breath: As the condition progresses, difficulty breathing, especially during physical activity or when lying flat, may occur. This symptom is often accompanied by a sensation of breathlessness.
Heart Palpitations: Irregular or rapid heartbeats, known as palpitations, can occur in individuals with Mitral Stenosis. These palpitations may be felt as a fluttering sensation in the chest.
Chest Discomfort: Some individuals may experience chest discomfort or a tight, heavy sensation in the chest. This symptom can vary in intensity and may be triggered by exertion or emotional stress.
Coughing: Mitral Stenosis can cause a chronic cough that is typically worse at night or when lying down. Wheezing or a whistling sound when breathing may also be present.
Swelling: Swelling in the ankles, feet, or abdomen, known as edema, can occur due to fluid retention caused by Mitral Stenosis. This swelling is often more prominent at the end of the day.
Fainting or Dizziness: In some cases, Mitral Stenosis can lead to episodes of fainting or dizziness. These symptoms occur due to decreased blood flow and inadequate oxygen supply to the brain.
Frequent Respiratory Infections: Individuals with Mitral Stenosis may be more susceptible to respiratory infections, such as bronchitis or pneumonia, due to compromised lung function.
Cyanosis: In severe cases of Mitral Stenosis, a bluish discoloration of the lips, fingertips, or skin (cyanosis) may occur. This indicates inadequate oxygenation of the blood.
Reduced Exercise Tolerance: As the condition progresses, individuals may notice a decline in their ability to engage in physical activities or exercise due to increased fatigue and shortness of breath.
Treatment for Mitral Stenosis
Recognizing these signs and symptoms of Mitral Stenosis is crucial for early diagnosis and timely medical intervention. If individuals experience any of these symptoms, it is important to consult a healthcare professional for a comprehensive evaluation and appropriate management.
Managing Mitral Stenosis (MS) involves a comprehensive approach aimed at alleviating symptoms, improving heart function, and preventing complications.
The treatment options for Mitral Stenosis vary depending on the severity of the condition and individual patient factors.
Here are some common treatment approaches:
Medications
Medications play a significant role in managing Mitral Stenosis. Diuretics may be prescribed to reduce fluid buildup and relieve symptoms of edema. Blood thinners, such as anticoagulants, may be recommended to reduce the risk of blood clots and stroke. Additionally, medications to control heart rate, rhythm, and blood pressure may be prescribed as necessary.
Non-surgical Procedures
In some cases, non-surgical interventions may be used to alleviate Mitral Stenosis. Balloon Valvuloplasty is a minimally invasive procedure where a balloon-tipped catheter is inserted into the narrowed mitral valve and inflated to widen the opening, improving blood flow. This procedure can provide significant relief of symptoms and improve heart function.
Surgical Interventions
Severe cases of Mitral Stenosis may require surgical intervention. Mitral Valve Repair or Replacement is performed to restore or replace the damaged mitral valve. Valve repair aims to preserve the patient's valve, while valve replacement involves replacing the diseased valve with a mechanical or biological prosthesis. The choice of procedure depends on several factors and is determined by the healthcare team in consultation with the patient.
Lifestyle Modifications
Making certain lifestyle changes can help manage Mitral Stenosis. Following a heart-healthy diet, low in sodium and saturated fats, can reduce fluid retention and maintain optimal blood pressure. Regular exercise, as recommended by a healthcare professional, can help improve overall cardiovascular fitness. It is also important to avoid smoking and limit alcohol consumption to support heart health.
Regular Follow-up with Doctors
Individuals with Mitral Stenosis require regular medical follow-up to monitor the progression of the condition, evaluate symptoms, and adjust treatment as necessary. This may involve periodic echocardiograms, electrocardiograms (ECGs), and other diagnostic tests to assess heart function and identify any changes.
Treatment approaches for Mitral Stenosis aim to improve symptoms, prevent complications, and enhance overall quality of life. The choice of treatment depends on individual factors and should be discussed with a healthcare professional to ensure personalized and effective management.
Conclusion
Mitral Stenosis is a significant cardiac condition that requires proper understanding, timely diagnosis, and appropriate management to improve patient outcomes. By familiarizing ourselves with the causes, symptoms, diagnostic procedures, and treatment options discussed in this article, we can enhance awareness and promote early intervention.
It is crucial for individuals at risk, healthcare professionals, and the broader community to work together in preventing, detecting, and managing Mitral Stenosis effectively. Through ongoing research and advancements in medical science, we can continue to improve the quality of life for individuals living with this condition and strive for better outcomes in the future.