A portion of the body can become completely or partially senseless. Often, tingling or burning is present along with sensory loss or paralysis. This sensation can make it difficult to identify specific body parts and includes...
A portion of the body can become completely or partially senseless. Often, tingling or burning is present along with sensory loss or paralysis. This sensation can make it difficult to identify specific body parts and includes the following:
Temperature Pain Light Touch Vibration
Many times, numbness is innocuous and transient. Serious medical conditions that call for the proper treatment to alleviate the problem can cause severe instances of numbness.
What Makes Me Numb?
When nerves are harmed, agitated, or compressed, numbness is a sign that results. There are several conceivable justifications for this, containing but not restricted to:
- Disorders of the nervous system or brain
- Neuropathy
- Stroke
- Herniated Disc with Brain Tumour
- Spinal Cord Damage
- Gilles de la Tourette Syndrome
- Overuse or Trauma-Related Injury
- wrist pain
- Frostbite
- Chronic Illnesses
- Several Sclerosis
- Diabetes
- Alcoholism
- Virus and Infections
- Lyme
- Syphilis
- Shingles
- Crisis Medical Attention
You are instructed to seek instantaneous medical aid if you feel numb:
- Affects A Whole Bodily Part, Such As A Whole Side, Arm, Or Leg.
- Spreads To Different Parts Of The Body Appearance In The Genital Region, Buttocks, Or Thigh
- Confusion
- Incontinence
- Paralysis
- Problems Speaking Problems Seeing
- Difficulty Breathing
- Unconsciousness
Impaired Sensation
People depend on touch to quickly remove themselves from a hot object or feel changes in the ground beneath their feet. Sensations are what we refer to as the impaired
The impaired sensation is the term for when you don't feel as well, particularly with your hands or feet. If your sensation is impaired, you might not experience anything at all. Or you might experience strange feelings like:
- Numbness
- Tingling
- Weakness
- Pain
- Sensational Impairment Can Cause Harm And Equilibrium Issues.
It might be a short-term occurrence following an injury or a chronic condition brought on by diabetes or another disease. An unexpected loss of feeling can be life-threatening.
What contributes to decreased sensation?
You've had impaired sensation if you've ever crossed your knees and had one of them go numb. While this sensation might disappear in a few minutes, other conditions that impede sensation might be impaired
The impaired sensation can be for several including:
- Joint patumorin tumor
- Palmar-plantar syndrome
- Disease of Charcot-Marie-Tooth
- Persistent renal failure
- Delirium
- Diabetes
- The condition of Guillain-Barré
- Brain damage
- Lead poisoning from a herniated spine
- Peripheral neuropathy due to opioid reliance
- Phantom after an amputation, limb discomfort
- Stroke sciatica shingles spinal nerve injury
- Pulsatile ulnar nerve
When should I get medical attention for an affected impairment?
Because sudden loss of sensation could be a sign of a stroke, it can be a medical crisis.
If you or someone you care about exhibits any of the following indications, get medical help right away:
- Equilibrium is lost
- Abruptly confused
- Unknown source of an abrupt, severe headache
- Difficulty seeing, abrupt weakness on one side of the body
Inform your healthcare provider if your impaired sensation symptoms appear to be growing worse if you are collapsing or losing your balance as an outcome of your impairment, or if you are encountering any other of these signs.
Bad and good symptoms
Positive and negative abnormal sensory sensations can be together. The prototypical positive symptom is tingling (pins and needles); other positive sensory phenomena include itching and altered sensations that are depicted as pricking, bandlike, lightning-like shooting feelings (lancinations), aching, knifelike, twisting, drawing, and pulling. These indications continually hurt.
Positive phenomena typically arise from impulse trains produced at locations along a central or peripheral sensory route with elevated excitability or sites with threshold thresholds. According to the quantity, frequency, timing, distribution, and type of ectopic impulses as well as the kind and function of the nervous tissue in which they originate, the character and intensity of the abnormal feeling will vary. Positive occurrences do not always appear to be accompanied by a sensory deficit (loss) on inspection because they signify excessive activity in sensory pathways.
Negative photos reflect the loss of sensory Functional characterized acterised by diminished or absent feeling, which is frequently felt as numbness, as well as by abnormal results on sensory examination. In disorders of peripheral sensation, at least 50% of the afferent axons innervating a specific location are likely lost or inactive before a sensory deficit is visible on a clinical examination. Even though few fibers are functioning, a lack of cutaneous feeling may go unnoticed by the patient and be difficult to demonstrate on examination if the rate of loss is gradual. If it is rapid, however, both positive and negative phenomena are typically obvious. Studies of sensory nerve conduction or somatosensory-evoked potentials may be able to detect subclinical levels of sensory impairment.
Sensation Clinical Examination
Primary sensation evaluations make up the majority of the sensory examination. (Discomfort, touch, palpitation, joint position, and thermal feeling). Interpretation is made more difficult because the examiner must rely on the patient's answers. In some indie visuals, the examination may be restricted. For instance, sensory examination in a comatose patient is limited to watching the rapidity of withdrawal in reaction to a pinch or other noxious stimulus. It is crucial to compare the two parts of the body's reactions. It might not be possible to examine cutaneous sensation in an awake but uncooperative patient, but it is possible to get a sense of proprioceptive function by observing how well the patient performs movements that call for balance and accuracy.
Testing should be done on the affected area in patients who have sensory complaints until the normal feeling is abnormality distribution is described and contrasted with root and peripheral nerve regions. Some patients have sensory complaints that are localized anatomically and are accompanied by gross inconsistencies or by neither abnormalities nor abnormalities on inspection. The examiner should think about whether the sensory complaints are a covert cry for assistance with situational or psychological issues.
Initial Sensation
Typically, a clean pin is used to evaluate one's perception of pain before being discarded. The patient is advised to shut their eyes and concentrate on the stimulus's stinging or unpleasant quality rather than just the pressure or touch feeling it produces. By moving radially outward from the most hypoalgesia location, areas of hypoalgesia should be mapped. The easiest way to evaluate temperature perception for both hot and cold is with small containers filled with water that is the desired temperature. A tuning fork or other metal item that is at room temperature can be touched to the skin to test for areas of a sense of a cold sensation. Holding an object made of metal under warm water that has been heated to the desired temperature can be used to evaluate warm temperatures.
Because various receptors react to cold and warmth differently, it is important to test one's appreciation of both. A wisp of cotton or a delicate camel hairbrush is typically used to evaluate the pressure on the skin. The abundance of sensory endings that encircle each hair follicle makes it generally preferable trying a trying touch on hairy skin. The patient is tested while keeping their eyes closed, and they are expected to signal the position of the stimulus as soon as they become aware of it.
Sensory Quantitative Testing
Commercially accessible tools for sensory testing are efficient. For the serial evaluation of cutaneous sensation in clinical trials, quantitative sensory testing is especially helpful. The most popular application involves threshold testing for temperature, vibratory, and touch sensations.
Cerebral Sensation
The evaluations for graphesthesia and stereognosis as well as two-point discrimination, touch location, bilateral simultaneous stimulation, and cortical function are the most frequently used. When a patient is aware and cooperative and these sensory tests are abnormal, it usually means that the parietal cortex or thalamocortical projections have been damaged.
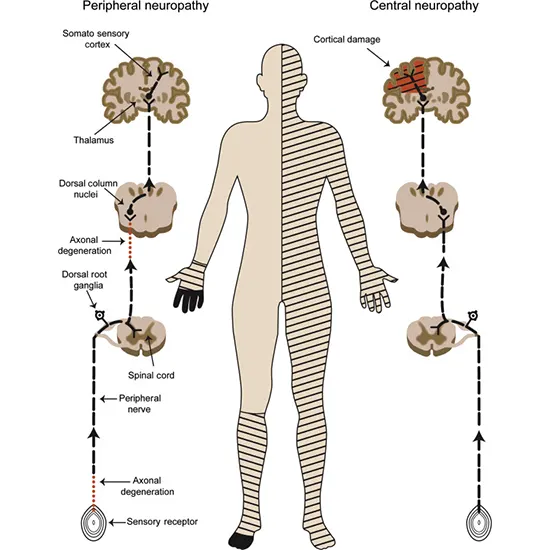
Localization of sensory abnormalities
Lesions at numerous layers of the nervous system, from the parietal brain to the peripheral sensory receptor, can cause sensory symptoms and signs. The most crucial step in identifying their source's location is to take note of their character and distribution. The main findings are their size, arrangement, symmetry, character, and severity.
Dysesthesias without sensory examination results can be challenging tingling dysesthesias in the acral distribution (hands and feet) can have a systemic cause, such as secondary to hyperventilation or a drug like acetazolamide. Distal dysesthesias can precursor to a precursor as that caused by a vitamin B12 deficiency, or they can be an early symptom of a developing polyneuropathy. Distal dysesthesias can occasionally have no known cause. A lesion at that location is indicated by dysesthesias, on the other hand, whose spread matches that of a specific peripheral nerve structure. For instance, dysesthesias confined to the fifth finger and the nearby fourth finger half on one hand consistently indicate ulnar nerve disorder, most frequently at the elbow.
Sensory neuropathy
A widespread, asymmetric sensory loss that can appear proximally or distally and, in the limbs, legs, or both is known as sensory neuronopathy (or ganglionopathy). This sensory loss is not length dependent. With time, pain and numbness develop into sensory ataxia and impairment of all sense modalities. This disorder is typically idiopathic, paraneoplastic, or connected to an autoimmune disease, especially Sjogren’s syndrome.
When the top level of the sensory loss extends to the trunk, there is a higher likelihood that a spinal cord lesion will result in numbness or paresthesia in both feet unless a peripheral neuropathy is to blame, the lesion that causes all affected limbs is likely in the cervical area or brainstem. An upper motor neuron lesion is supported by the presence of these signs, and the degree of involvement may be indicated by a hyperesthetic band on the trunk.
How are sensory impairments identified?
Your healthcare provider may begin by asking you a series of inquiries to determine the nature and extent of your sensory impairment, such as the following:
- Where do you notice the shift in feeling? Do you sense it across the top of your skin or farther down?
- When do novel sensations or a loss of sensation typically occur? Do they remain throughout the day or do they appear and go?
- Do activities like resting, moving, or sleeping make your conditions feel better or worse?
- Then, they frequently conduct a physical check. To gauge how much you can feel, they might gently tap on your skin.
They might also suggest one or more of the procedures listed below:
Nerve conduction velocity studies, which gauge how well electrical impulses travel through your nerves, imaging scans like computed tomography (CT) or magnetic resonance imaging (MRI) to look for damage or abnormalities in your brain, spine, or other areas, and reflex tests
Treatment & Diagnosis of Numbness
Your physician will have to understand all of your signs, go over your medical record, and perform a physical order to specify the basis of your numbness. An MRI or CT scan can provide information about the location and nature of the impacted nerves. In addition to nerve conduction tests, a blood test may be required.
The purpose of therapy is to remedy the illness that is the source of the numbness. Depending on your unique situation, this will change. One or more of the following will most certainly be part of the treatment:
- Drugs for Nerve Pain
- Dietary and lifestyle adjustments
- Physical Exercise
- Surgery
How are sensory impairments managed?
Depending on the underlying cause of your impaired sensation, your doctor may suggest a different course of action.
The instantaneous paired feeling is frequently caused by diabetic neuropathy. If you have diabetic neuropathy, your doctor may give you advice on how to better control your blood sugar by monitoring it and taking medicine for high blood sugar.
Taking good care of your feet by getting your toenails cut at a podiatrist's clinic and scheduling routine foot exams can also be beneficial.
Surgery may help alleviate pressure on the nerve and improve your sensation if your impaired sensation is brought on by sciatica or a pinched nerve.
To help you handle the symptoms brought on by unusual sensations, your healthcare provider might also recommend painkillers.
The impaired sensations can be brought several number of diseases. Depending on the cause, your doctor may suggest a different course of action.
A stroke may be present if you experience a sudden lack of sensation. An immediate response is necessary for this medical catastrophe.