Oligodendrocytes are the source of oligodendrogliomas. Oligodendrocytes produce a material that shields and supports the operation of the brain. Myelin, a fatty white material produced by these cells, coats the neurons. Myelin...
Conquering Oligodendroglioma, one step at a time!
Introduction
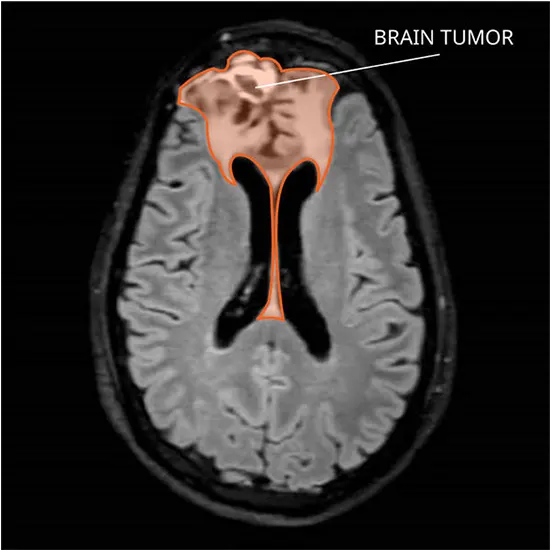
The tumour which forms in the brain is known as an oligodendroglioma. Rarely, these unusual tumours can occur in the spinal cord, albeit they typically grow in the frontal or temporal lobes of the brain.
Oligodendrocytes are the source of oligodendrogliomas. Oligodendrocytes produce a material that shields and supports the operation of the brain. Myelin, a fatty white material produced by these cells, coats the neurons. Myelin facilitates faster signal (impulse) transmission throughout the nerves.
The frontal lobe of the brain contains the majority of oligodendrogliomas. Although it is uncommon, they can also begin in the spinal cord.
Oligodendrogliomas may be benign or malignant. While many of these tumours develop more slowly, some do so. They might disseminate to different central nervous system regions. (brain and spinal cord). Typically, they don't expand outside the central nervous system.
Primary brain tumours are oligodendrogliomas. In the brain or spinal cord, primary brain tumours form. (Tumours that spread to the brain from another part of the body are called secondary brain tumours.)
What is the Presentation and location of Oligodendroglioma?
Oligodendroglioma typically appears as a somewhat well-circumscribed, variable-sized lump that can range in shape from round to oval. Low-grade diffuse astrocytoma is similar to oligodendroglioma in form, but oligodendroglioma has a distinctive predilection for the cortex.
It often affects the cortex and subcortical white matter and is superficially situated. On T2 fluid-attenuated inversion recovery imaging, cortical involvement is best seen as (extensive) cortical thickening. It is normal for the focus area to shrink, alter, or even erode the overlying cranium because of its periphery. The frontal lobe is the most typical site for tumours (50–65%), where they are most frequently found (85%) supratentorial.
Explore the Pathophysiology
Most frequently in the frontal lobes, but sometimes occasionally in the temporal and parietal lobes, OGs are located in the white matter of the cerebral hemispheres (80 to 90% supratentorial). With widespread infiltration across the surrounding white matter, the tumour is primarily found in the cortical-subcortical region. Although it is uncommon, OG has also been discovered to be intraventricular or subependymal.
Here is the Epidemiology
After glioblastoma and diffuse astrocytoma, OGs are the third most frequent primary brain tumour. They are rare, having a frequency of 0.2 per 100,000 people. Roughly 5% of all primary CNS tumours are OGs. Their male-to-female ratio ranges from 1.1 to 2, with one research reporting a ratio as low as 0.92.
A Taxonomy of Oligodendroglioma: Differentiating the Variants
- Oligodendroglioma of grade 2 (low grade): An oligodendroglioma is a benign (noncancerous) tumour that grows slowly and may do so for years before symptoms manifest. The majority of the time, this tumour doesn't spread and just affects the local tissue. However, Grade 3 fast-growing oligodendrogliomas are possible and call for more aggressive therapy.
- Oligoastrocytoma of grade 2 (low grade): This "mixed glioma" tumour is benign. Another variety of glioma (brain tumour) that arises from astrocyte glial cells is astrocytoma. Oligoastrocytomas can develop into malignant (cancerous) anaplastic oligoastrocytomas and contain both aberrant oligodendroglioma and astrocytoma cells.
- Anaplastic oligodendroglioma of grade 3 (high grade): The central nervous system of the body can be quickly affected by the rapid growth and spread of this malignant (cancerous) tumour. (CNS). vigorous treatment is necessary.
- Anaplastic oligoastrocytoma of grade 3 (high grade): This mixed glioma develops into an anaplastic oligoastrocytoma when abnormal astrocyte cells combine with abnormal oligodendrocyte cells. This form of tumour requires intensive therapy because it spreads quickly to other areas of the CNS and grows quickly.
Exploring the Origins and Risk Factors for Oligodendroglioma
There are a few risk factors for oligodendroglioma, yet the reason is still unknown:
- Age: Although brain tumours can develop at any age, the danger increases with ageing.
- Radiation exposure: Nuclear weapons exposure and radiation therapy used to treat cancer are two examples of ionising radiation.
- Glioma in the family history: Although a genetic component is uncommon, a family history of glioma might increase a person's risk by twofold.
- Genetics: Gene alterations that affect how cells function can result in cancer. Genes can modify (alter) throughout your lifetime.
Normal genes may become cancer-causing genes as a result of mutations. This aberrant cell has a high rate of multiplication, which promotes the growth and spread of cancer.
Certain environmental and lifestyle factors, such as exposure to chemicals, smoking, and food, can result in mutations. Other mutations appear to happen at random and have no recognised reason.
- Lifestyle: Even though you might not have an oligodendroglioma because of your lifestyle, making healthy lifestyle decisions like eating a balanced diet, quitting smoking, and exercising regularly can help you stay strong during treatment. Making healthy decisions is good for your overall health and well-being.
The Frequency of Oligodendrogliomas
Oligodendroglioma is uncommon. Every year, doctors in the US diagnose them in around 1,200 individuals. Approximately 4% of all initial brain tumours are oligodendrogliomas.
How much does Oligodendroglioma Spread?
Although it is rare, oligodendrogliomas can spread to other parts of the CNS through the cerebrospinal fluid (CSF). Rarely do oligodendrogliomas spread to other organs outside of the CNS.
Warning Signs :
The symptoms can overlap with those of other types of brain tumours or diseases and vary according to the location and size of the tumour. The following signs of oligodendrogliomas can occur:
- Seizures
- Headaches
- Personality or behaviour changes
- Weakness
- Partial blindness
- Language issues
Seizures are the most prevalent symptom, occurring in roughly 80% of patients at some time throughout the disease. Hemiparesis, as well as personality or behavioural problems, can result from frontal lobe tumours. Sometimes there are no symptoms at all for temporal lobe tumours. However, these tumours can cause seizures or linguistic difficulties if they are present.
Depending on the tumour's size and location, there may be other symptoms. A frontal lobe or temporal lobe oligodendroglioma can produce symptoms that are consistent with the interruption of normal function in those regions.
For instance, the frontal lobe of the brain is in charge of a variety of intricate processes like personality, behaviour, logic and thinking, and movement control. Accordingly, the following signs and symptoms may be brought on by tumours in this area of the brain:
- A personality change
- Alterations in behaviour
- A lack of strength or difficulty moving the body
What are the Problematic Consequences of Oligodendroglioma?
The following are oligodendroglioma complications:
- Hydrocephalus (build-up of fluids in the brain, often caused by the tumour blocking the flow of cerebrospinal fluid) intracranial bleeding
- Recurrence (return of the tumour)
- Parkinsonism (abnormal movement patterns frequently present in Parkinson's disease)
- Surgery, chemotherapy, and radiation therapy may cause side effects and difficulties for certain patients.
Potential Diagnoses:
Anaplastic oligodendroglioma is the most significant oligodendroglioma differential diagnosis. As will be discussed below, conventional imaging cannot consistently distinguish between these cancers of different World Health Organization (WHO) grades.
- Other tumours including low-grade diffuse astrocytoma, ganglioglioma, dysembryoplastic neuroepithelial tumour, and pleomorphic xanthoastrocytoma are included in the differential diagnosis on imaging.
- Although the latter three share a cortical distribution with oligodendroglioma and ganglioglioma shares calcification as a prominent characteristic, all three of these tumours often affect a younger patient population.
- Anaplastic oligoastrocytoma imaging findings resemble those of anaplastic oligodendroglioma, just like with low-grade tumours, making it difficult to accurately distinguish between the two on CT or MRI. Anaplastic oligodendroglioma frequently shares imaging characteristics with oligodendroglioma, although standard imaging cannot reliably predict the cancer grade.
According to histological results, anaplastic oligodendroglioma exhibits oedema, haemorrhage, cystic degeneration, and contrast enhancement more frequently than oligodendroglioma. Ring-like contrast enhancement, which is typically linked with glioblastoma, can occasionally be noticed.
What are the Expected Lifespan and Survival Rates?
Compared to most other brain tumours, oligodendrogliomas have a better prognosis. There are numerous treatment options, and oligodendrogliomas seem to respond favourably to therapy. While it is uncommon to be able to cure oligodendroglioma fully, it is entirely doable to extend a patient's life.
The grade of the tumour and the timing of the diagnosis both affect the oligodendroglioma patient's life expectancy. It's crucial to keep in mind that every person's circumstances are unique, and life expectancy numbers do not account for specifics like your general health and the standard of treatment you receive.
People with grade II oligodendrogliomas typically live for about 12 years after being diagnosed. The average life expectancy for those with grade III oligodendrogliomas is 3.5 years.
Assessment Findings:
- Neurological examination: During a neurological examination, it is possible to learn whether a tumour may be present and which area of the brain may be impacted.
- Imaging tests: Imaging examinations assist in locating and sizing the brain tumour. Brain tumours are frequently diagnosed using various magnetic resonance imaging (MRI) procedures. Computed tomography (CT) and positron emission tomography (PET) are two other imaging tests that may be performed.
- Biopsy: Before surgery, a sample of the tumour or suspicious tissue is obtained, transported to a lab, and examined to determine the cell types present and how aggressive (rapid spreading) they are. A small sample of the damaged tissue is removed during a biopsy using a needle.
- Other special tests: Important information regarding the types of mutations (changes) the tumour cells have undergone can be obtained through another specialised testing of the tumour cells. This information is useful for determining a prognosis (disease outcome and course) and directing therapy choices.
What are the Healing Protocols of Oligodendroglioma?
The location, size, and grade of the tumour all influence the course of treatment for oligodendroglioma. Your medical choices could consist of:
- Surgery: When an oligodendroglioma appears in a location that may be reached by doctors, the tumour is removed. They take great care to minimise any collateral damage to the surrounding healthy tissue while gently removing the tumour. Sometimes, a single surgical procedure cannot eliminate the tumour.
- Radiation therapy: After surgery, the tumour's remaining tissue is destroyed with high doses of X-rays administered by cancer experts known as radiation oncologists. In this radiation therapy is most helpful.
- Chemotherapy: Cancer cells throughout the body are eliminated by anti-cancer medications. Most chemotherapy is administered as an injection into a vein or as a tablet. To eliminate cancer cells that may have survived surgery or radiation, doctors may advise chemotherapy either before or after the treatment.
- Clinical trials: You and your healthcare practitioner may choose to consider clinical trials if all other treatments have been tried and failed.
New Therapies of Oligodendroglioma:
- Targeted drug therapy focuses on particular aberrations that are prevalent in cancer cells. Bevacizumab (Avastin), which is used to treat glioblastoma, is one instance.
- Pumps used in convection-enhanced delivery (CED) administer chemotherapy or other targeted medicinal therapies to a tumour continuously.
- Electric fields are delivered to the brain by tumour-treating fields (Optune). The development of cancer cells may be halted by these fields. Adults with newly discovered glioblastoma are treated with temozolomide with Optune, a portable, wearable device.
- With implanted, biodegradable therapy (Gliadel), chemotherapy is delivered to any remaining tumour tissue that cannot be surgically removed. Using particles with an abnormally high surface area, nanoparticle therapy transports chemotherapy over the blood-brain barrier.
Wellness Support
Palliative care, which is not a form of treatment, focuses on easing tumour-related symptoms. Along with serving as an additional support team for the other members of the treatment team, palliative care professionals work to relieve pain and other symptoms. When receiving treatment, especially more invasive forms including surgery, chemotherapy, and radiation therapy, palliative care is frequently used.
What is the Prognosis of Oligodendroglioma?
People with oligodendroglioma have a wide range of prognoses. The location and grade of the tumour, as well as your age and general health, can all have an impact on the prognosis.
Oligodendroglioma can often be successfully treated by medical professionals. To completely remove the tumour and guarantee that it won't grow back, patients occasionally require many operations. With these tumours, some people lead active, symptom-free lives.
To prevent the tumour from developing or spreading, persons with oligodendroglioma occasionally need to continue receiving therapies like chemotherapy or radiation. These therapies might go on forever.
You should continue to see your doctor after oligodendroglioma treatment for the rest of your life. Your doctor can keep an eye out for any new tumour growth in you and can start treating you immediately soon.
Strength and courage in the face of Oligodendroglioma!









