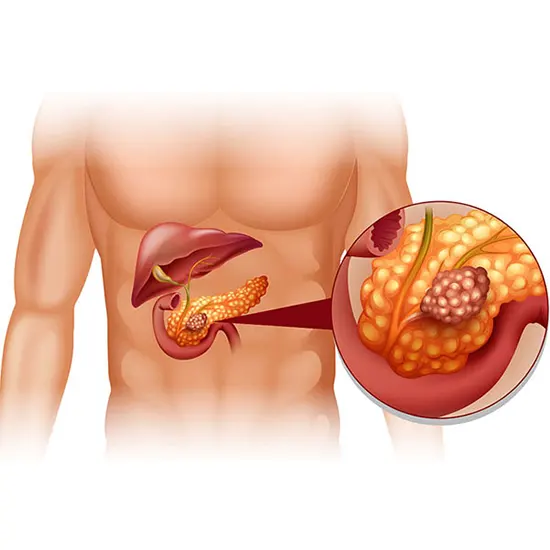
Pancreas is an organ that is present in the upper part of the abdomen behind the stomach and plays an important role in providing energy to the body cells to carry out various functions. The pancreas acts both as a gland as...
Introduction
Pancreas is an organ that is present in the upper part of the abdomen behind the stomach and plays an important role in providing energy to the body cells to carry out various functions.
The pancreas acts both as a gland as well as an organ. It is characterized as an organ because it releases certain substances in the body.
As an exocrine gland it is involved in the production of certain enzymes that aid in digestion of the food. It also regulates the hormone that regulates blood glucose levels and thus acts as an endocrine gland.
What Are the Types of Pancreatitis?
The two forms of pancreatitis are acute and chronic.
Acute pancreatitis: this type of inflammation is usually sudden in nature and usually lasts for a short period of time. It may begin as a slight discomfort in the body but may ultimately progress into a life-threatening disease.
The common symptoms that may appear are bleeding, and damage to the pancreatic tissue. The infection may further progress to harm other vital organs which are the kidneys, the heart and the lungs.
Chronic pancreatitis: it usually occurs as a sequel of acute pancreatitis and has a longer period of effect as compared to acute pancreatitis. The most common etiological factor of chronic pancreatitis is excessive alcohol control over a very long period of time. Alcohol consumption doesn't show any instant effects but ultimately when done over a long period can be deleterious or even fatal.
Idiopathic pancreatitis: these are cases of pancreatitis where the examiner fails to identify the cause of pancreatitis as there are no absolute findings through the history recorded from the patient, histological or serological tests, physical examination, ultrasound of the abdomen, or any laboratory tests.
In these cases, pain develops in the left part of the abdomen and may be seen radiating to the back of the patient. The patient describes the pain as excruciating or burning and the pain usually comes and goes. Any firm etiological factor becomes very difficult to be identified by the examiner. It may continue for several hours and can even last for several days.
Causes
When there is any discrepancy in the distribution of the enzymes produced by the organ, the enzymes remain grounded or stored in the pancreatic tissue and thus cause inflammation thereby causing irritation to the cells.
Thus problems arise in the digestion process of the body. There may even be the production of necrosed tissue in the organ.
There are various conditions that can ultimately lead to pancreatitis. These conditions are as follows:
- Presence of gall stones in the duct
- Chronic alcohol abuse
- Certain medications
- Any surgery of the abdomen
- Any trauma or injury to the abdomen
- Cancer to pancreas
- Obesity
- Hyperglycemia which is due to impaired function of the parathyroid gland
- Cystic fibrosis
Pathophysiology
The process of infection begins from localized irritation and ultimately leads to an aggressive inflammatory process which is usually systemic. Inside the acinar cells there is premature activation of the enzyme trypsinogen into trypsin which increases the ductal pressure. The pH and calcium homeostasis begins to disrupt and ultimately toxins are released and thus excessive tissue damage is seen.
Individuals with certain genetic predispositions to this disease usually have acute attacks over a prolonged period that progresses into chronic pancreatitis.
Symptoms
The signs and symptoms of pancreatitis vary, depending on which type of pancreatitis from which the individual is suffering
Acute pancreatitis includes:
- There is pain in the upper abdominal region
- The pain may radiate to the back of the patient
- Pain and tenderness in the abdomen
- Nausea and vomiting
- Increased pulse rate
- Fever
Chronic pancreatitis includes:
- Pain in the upper abdominal region
- The pain severely aggravates after eating
- Unintended Weight loss
- smelly and oily stools
When to see a doctor?
You should always remember that your life is important to you and for all the people around you. So seeking medical help is a necessity. If you encounter any of the symptoms mentioned you should immediately see a doctor and seek treatment for the same.
Risk factors
There are certain risk factors that are associated with increased chances of the development of pancreatitis. These risk factors are :
- Chronic alcohol abuse: Heavy drinkers, that is people who consume five to six drinks a day, have an increased risk of pancreatitis.
- Obesity: obese individuals are generally at a high risk to get affected by pancreatitis.
- Smoking cigarettes: cigarette smokers are at a very high risk as compared to the non -smokers.
- Diabetes: it has a severely damaging effect on the pancreas thus putting the individual at an increased risk.
- Genetics: Family history also plays a crucial role.
Complications
- Damage to the kidneys: Acute pancreatitis usually causes severe kidney damage which has to ultimately be treated through dialysis.
- Infection: it makes the pancreas more susceptible and prone to other bacteria and infection.
- Diabetes: As the function of the pancreas of maintaining blood sugar levels are affected so it can cause diabetes in some patients leading to hypoglycemia.
- Respiratory problems: it can cause chemical changes in the lungs affecting the breathing process causing the oxygen levels to fall critically low.
- Compromised nutrition: as the amount of enzymes being secreted by the pancreas is less during pancreatitis thus the nutrition of the individual is compromised. You may be eating healthy foods in good amounts but that won't be utilized by the body due to a deficiency of the enzymes by the pancreas.
Diagnosis
The tests and procedures that can be done for diagnosing pancreatitis are:
- Blood tests: blood tests report highly elevated levels of pancreatic enzymes along with liver enzymes and white blood cells can indicate pancreatitis.
- Stool tests: more the amount of fat observed in the stools more is the disruption in the normal digestive processes.
- MRI: will show abnormalities in pancreas and its ducts and in the liver.
- CT Scan: it is used for the identification of the presence of gall stones and also shows the extent of pancreatic inflammation.
- Ultrasound: of the abdomen will also depict the pancreatic inflammation and the presence of gallstones.
Treatment
More liquid food or fluids are suggested to be consumed by the patient in the early days of pancreatitis allowing the pancreas to have a good amount of time to recover.
As soon as the inflammation subsides patients can start following their normal diet pattern.
If the symptoms of the inflammation still persist and there is difficulty in consuming food then a feeding tube can be of great advantage for feeding purposes and thus obtaining nutrition.
Medications for pain: pancreatitis causes a considerable amount of pain to the patients. Thus intravenous fluids are most recommended. Dehydration is very common in patients being treated as the pancreas uses a great number of fluids for its recovery. Thus more and more fluids should be administered.
Pancreatic surgery: in some cases it may be performed to remove the inflamed or necrosed tissue of the gland with endoscopy to provide relief to the patient.
Surgery of the gall bladder: If the understood cause for the pancreatitis is the presence of gall stones. In those instances, the removal of gallstones is usually recommended by doctors to provide relief from the symptoms.
Changes in the medications: If any medication already being consumed by the patient is causing damage to the pancreas and inflammation then it should be immediately discontinued or any alternative medication should be discussed and provided to the patient.
Treating alcohol dependence: consumption of alcohol for over long periods of time is damaging not only to the pancreas but to all the other glands and organs of the body. The concept of rehabilitation centers can be discussed with the patients and their families and thus support and assistance can be provided to them.
Artificial enzymes: in long-standing cases of pancreatitis the nutrition of the patient is severely compromised as the absence of enzymes makes it almost impossible to completely digest the food . Thus enzymes in artificial forms need to be taken along with the food so that it can be digested by the body.
Diet changes: A low-fat diet is usually recommended.
Treatment for chronic pancreatitis
The treatment course for chronic pancreatitis can be divided into multiple phases. These phases are:
- Medical
- Endoscopic
- Surgical
Medical: Under these approaches different types of medications are employed to provide relief to the patient.
- A combination of analgesics and antidepressants is used .
- Patients are motivated to limit or rather discontinue alcohol consumption and cigarette smoking.
- Low fat meals and small portions are recommended.
- Insulin is injected in patients with diabetes.
- Supplements for some vitamins like A, D, E,K and B12 are given.
- Pancreatic enzymes are given in the form of proton pump inhibitors.
- Steroid therapy
Endoscopic
- Placement of stent is done to unblock the pancreatic ducts.
- Drainage of the pseudocyst is done
Surgical: Decompression and Resection are done. Sometimes the surgeon tries to identify and create a new passage for the flow of the contents of the pancreas so that the fluid can easily be drained.
Other procedures are:
- Whipple surgery
- Distal pancreatectomy
- Frey procedure
Whipple surgery involves removing only the head of the pancreas and leaving the body and tail part as such or intact.
In distal pancreatectomy, the tail and the body part of the pancreas are removed leaving the head of the pancreas as such.
In the Frey procedure there is a combination of resection of some part of the pancreas and simultaneous drainage is carried out for the fluids.
In some extreme conditions, the whole of the pancreas is removed.
Other Procedures Are:
- Puestow procedure
- Beger's procedure
In all the procedures the surgeon tries his best to remove the necrotic or inflamed part of the tissue and make the rest of the organ or gland able to perform its functions efficiently.
Nursing rationales
- The patient is never fed orally, only the fluids are administered to the patient through the intravenous route.
- A peaceful and resting environment should be provided to the patient.
- The stimulation to the Gastrointestinal system should be very less providing considerable time to the pancreas for recovery.
- There should be complete bed rest during an acute attack.
- Abdominal pressure and tension can be removed by changing the posture that is flexing the knees and sitting in an upright position.
- The patient should be engaged in some diversional activities like watching television, book reading or listening to the radio.
Prevention
- Limit the consumption of alcohol: the more alcohol abuse more is the release of toxins produce pancreatic damage. Thus limiting alcohol consumption will have a soothing effect on the body.
- Avoid smoking cigarettes: cigarette smoking makes an individual more prone and susceptible to getting infections in vital organs and glands.
- Regular exercise: people who have a sedentary lifestyle and are more into eating unhealthy foods are definitely more prone to infections or diseases as common to people who have an active lifestyle and eat healthy foods.
- Avoid fatty foods: the more fat content in the diet more are the chances of developing gall stones in the gall bladder that undoubtedly act as an underlying cause for pancreas.
- Don't skip meals: in order to lose weight people tend to skip meals or crash diets which ultimately stimulates the liver to produce cholesterol. More will be cholesterol levels, more the chances of their conversion into gall stones.
Prognosis
For acute pancreatitis
It is a serious condition and can be life-threatening in some cases but with proper medical help and assistance, people have been seen recovering completely and leading a normal healthy life.
For chronic pancreatitis
If the damage to the pancreatic tissue sustains for a longer period of time it gets converted to chronic pancreatitis. People suffer from unbearable pain and Gastrointestinal problems for the rest of their lives. In those cases doing the surgical procedure is the only resolution. The necrosed or inflamed tissue or the gall stones acting as an underlying cause need to be removed and pancreatic ducts are unblocked by placing stents.









