Rare conditions known as paraneoplastic neurological syndromes (PNS) are linked to cancer but are not brought on by the disease itself, metastasis, or side effects of treatment. Often, they are autoimmune. PNS frequently comes...
Introduction
Rare conditions known as paraneoplastic neurological syndromes (PNS) are linked to cancer but are not brought on by the disease itself, metastasis, or side effects of treatment. Often, they are autoimmune. PNS frequently comes before cancer symptoms appear. To diagnose and treat these illnesses, onconeural antibodies are crucial. Instead of a specific neurological condition, these antibodies are specific to the malignancy.
The central, peripheral, and autonomic nervous systems, among others, can all be impacted. Although there may be multiple systems involved, as in encephalomyelitis, it is possible for only one system, such as the cerebellum, to be affected.
The peripheral nervous system (PNS) was first described in the 19th century by a French physician named M. Auche, who did so in 1890 while describing the involvement of cancer patients in the PNS. In 1983, Greenlee and Brashear identified PCA-1 (Purkinje Cell Antibody 1) in two patients with ovarian cancer and paraneoplastic cerebellar degeneration. Since then, other symptoms and antibodies have been reported, and the number of them continues to grow daily.
What is the Pathophysiology of PNS?
Most PNS are autoimmune. The body starts an immune response when attempting to remove tumour cells, and this reaction may target healthy neurological structures. T-cells or antibodies might facilitate this. As a result, the majority of PNS symptoms are caused by an autoimmune assault that targets the nervous system and is brought on by onconeural antigens that are secreted into the peripheral lymphoid tissue by an undetected primary or recurring tumour. These individuals frequently have lymphocytic pleocytosis, higher protein, enhanced IgG production, and oligoclonal bands in their cerebrospinal fluid (CSF), suggesting immunological pathology.
The prevalence rate of PNS-
These illnesses' precise incidence and prevalence are unclear. PNS is a clinically uncommon condition. These abnormalities are more common in some cancers than others. For instance, 2-3% of individuals with neuroblastoma or small cell lung cancer (SCLC) and 30-50% of patients with thymoma and sclerotic myeloma may develop PNS. It is estimated that clinically incapacitating PNS affects 0.5–1% of all cancer patients.
Antibodies
The specificity for paraneoplastic syndromes is quite high when antibodies against onconeural antigens, such as Hu, CV2/CRMP5, Yo, and amphiphysin, are detected alongside a compatible neurological condition. Antibodies against neuronal cell-surface antigens, such as NMDA receptor antibodies, on the other hand, are syndrome-specific but can also appear in paraneoplastic and idiopathic cases. Most patients with paraneoplastic disorders have antibodies against onconeural and/or neuronal cell-surface antigens in their serum and/or CSF. In a large European network research, only 80% of patients—even those with confirmed paraneoplastic syndromes—carried onconeural antibodies. With the identification of additional onconeural antibodies, this percentage is anticipated to rise in the future; yet, in clinical routine, seronegative cases frequently provide a significant diagnostic issue.
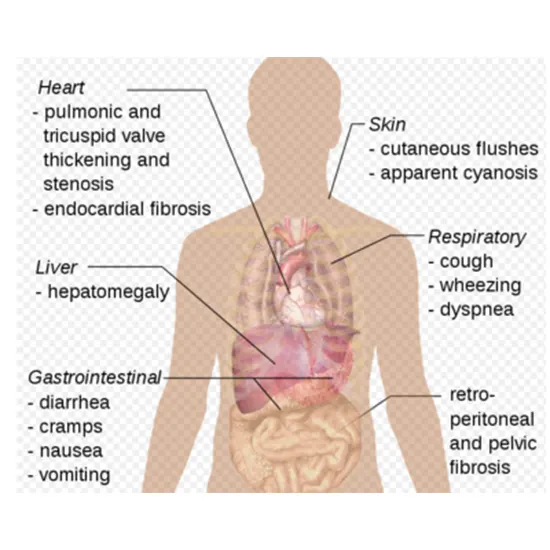
What are the Physical Manifestations of Illness?
Every component of the nervous system is susceptible to paraneoplastic neurological disorders. PNS-related symptoms may indicate that a particular nervous system structure is implicated. The sickness usually progresses subacutely and may result in a permanent loss of nervous system function.
Paraneoplastic diseases of the nervous system can show signs and symptoms rather fast, frequently over days to weeks. Before cancer is identified, paraneoplastic disorders of the nervous system frequently show signs and symptoms-
Depending on the body part affected, there may be a variety of signs and symptoms, such as:
- Have trouble walking.
- Difficulty keeping your equilibrium.
- Muscular coordination loss
- Muscular wasting or weakening
- loss of fine motor abilities, including the ability to pick things up
- Having trouble swallowing
- Speech that is slurred or stammers.
- Loss of memory and other cognitive problems
- Vision issues
- Disruptions in sleep
- Seizures
- Hallucinations
- Irrational and unusual movements
The most prevalent neurological paraneoplastic disorders
1. Limbic encephalitis
2. Subacute cerebellar degeneration
3. Opsoclonus-myoclonus
4. Lambert-Eaton myasthenic syndrome
5. Dermatomyositis
6. Cerebral ataxia
7. Stiff person syndrome
Limbic Encephalitis
The first neurological condition to be recognised and documented with a known malignant aetiology was limbic encephalitis (LE). Onconeural antibodies are currently used to distinguish between two forms of this disease: paraneoplastic and idiopathic. Women with ovarian teratoma are most affected by LE syndrome, which is most frequently associated with an elevated expression of anti-NMDA receptor antibodies. Small-cell lung cancer is the second tumour that is very closely linked to LE. According to Alamowitch et al., 50% of patients with limbic encephalitis and SCLC displayed antibody-positive reactions, typically with anti-Hu antibodies being present.
Symptoms of LE
As a result, the clinical condition is dominated by the signs of injury to these structures. The age of the patient and the disease's severity both affect how severe the symptoms are. Typically, subacute rather than acute illness onset occurs. Observed symptoms include.
- Short-term memory loss,
- Emotional lability,
- Psychosis, and
- Localised or generalised epileptic convulsions with consciousness abnormalities.
These include dyskinesias, paresis, and autonomic abnormalities in addition to respiratory failure as the disease progresses. Convulsions and motor abnormalities in children are more prevalent than in adults.
Subacute cerebellar deterioration
Purkinje cells in the cerebellar cortex are impacted by the neurological condition known as subacute cerebellar degeneration (SCD). Large, multipolar neurons called Purkinje cells oversee information processing and transmission. Women with breast or ovarian cancer are more likely to develop paraneoplastic SCD, which is most frequently linked to an elevated level of anti-Yo antibodies. Patients with small cell lung cancer, Hodgkin's lymphoma or urinary bladder cancer may also experience SCD symptoms. The disease typically starts severely.
Symptoms of SCD
- Progressive ataxia (motor impairment) of the feet and limbs, nausea, vertigo, and double vision are some of the symptoms.
- Speech is sluggish, aphonic, and unclear. The symptoms change as the illness progresses.
- Disorders in memory and swallowing may be seen.
Syndrome of opsoclonus with myoclonus
A paraneoplastic illness called Opsoclonus-Myoclonus Syndrome (OMS) develops as a result of an autoimmune process that affects the nervous system. 2-3% of children with neuroblastoma exhibit the illness. Studies have also suggested a link between OMS and celiac disease. Opsoclonus-myoclonus syndrome in adults is extremely uncommon and typically presents as the first clinical sign of breast, lung, or ovarian cancer.
Additionally, this illness might also be idiopathic, making brainstem encephalitis, metabolic, or toxic problems less likely to be associated with it. The disease usually has a subacute course. Opsoclonus and myoclonus are the disease's primary symptoms.
Symptoms of OMS
- Fast eye movements are associated with spontaneous, irregular, multifactorial, and opsoclonus syndrome.
- High frequency (10–15 Hz), big, and varied amplitude are traits of Eye motions. Involuntary, fleeting cramping of one or more muscles
- Lethargy, irritability, strabismus, cerebellar ataxia, and aphasia are some more signs.
Lambert-Eaton myasthenic syndrome (LEMS)
The disease Lambert-Eaton myasthenic syndrome (LEMS) is characterised by an issue with the nerve impulses' transmission from the neurological system to the skeletal muscles. The calcium channels in the presynaptic membrane's improper function are the cause of this illness. A small cell lung cancer or large intestine tumour is the most common malignant tumour which develops in around 60% of cases, while it can also happen in the course of other diseases (breast, prostate, stomach cancer). The illness typically appears after the age of 40, and its symptoms frequently appear before a cancer diagnosis. LEMS shares an autoimmune history with other paraneoplastic neurological disorders.
Symptoms Of LEMS
- Proximal skeletal muscular weakness, particularly in the thighs and arms, predominates among the clinical signs (muscle fatigue).
- The patient has issues raising his hands and ascending steps.
- There is an exaggeration of the patellar and ankle jerk reflexes.
- Autonomic problems (dry mouth, difficulty swallowing, orthostatic hypotension, impotence), paresthesia, and occasionally cerebellar ataxia are additional symptoms.
- High temperatures, hot baths, or illnesses may make the syndrome's symptoms worse.
Dermatomyositis (DM)
Dermatomyositis (DM) is an inflammatory condition that causes skin changes such as erythema and oedema that are primarily found on the face and limbs, as well as alterations to the muscles of the shoulder and pelvis (proximal myopathy). Dermatomyositis is accompanied by internal organ neoplasms in roughly 50% of cases in adults over 40. Ovarian, lung, stomach, pancreatic, and Hodgkin's cancer risk is enhanced. Dermatomyositis frequently occurs before the proliferative process, which is discovered later.
Symptoms of Dermatomyositis
High temperature and generalised muscle weakness are typical symptoms of the illness.
- Patients struggle to get up, perform squats, and ascend stairs without raising their hands vigorously.
- The first skin sympathiser is frequently basheerema (especially the orbital region and eyelids).
- The neck and chest were affected by the erythema patches and urticarial outbreaks.
- The so-called shawl symptom is created when erythema patches and urticarial eruptions expand to the neck and collar.
- There are flat, bluish lumps, erythema, and telangiectasia.
- Gottron's symptoms are on the hands' skin above the tiny joints.
- The nail ducts contain petechiae and erythematous lesions.
- The skin on the hand could become hard, earning it the nickname "mechanic's hand." In the subcutaneous tissue, there is also evidence of alopecia with exfoliation and calcium deposits (most commonly in joints).
When the illness worsens, speech, swallowing, and breathing issues arise, and the patient's overall health deteriorates and becomes more serious.
Brain deterioration (cerebellar ataxia)
This is the degeneration of nerve cells in the part of the brain that regulates balance and muscle movement (cerebellum). Unsteady or impaired walking, a loss of muscular coordination in your limbs, an inability to keep proper boot alignment, nausea, dizziness, involuntary eye movements, double vision, difficulties speaking, or trouble swallowing are just a few signs and symptoms that you may experience.
Rigid personality disorder
This illness, once known as "stiff man syndrome," is characterised by gradual, extreme muscle stiffness or rigidity, primarily affecting your legs and spine. Intense muscle spasms may also result from it.
Evaluation of pns
Physical examination
A basic physical examination and a neurological examination will be performed by your doctor or a neurologist. He or she will quiz you and run quick tests in the office to determine:
- Reflexes
- muscular power
- The tone of muscles, touch, vision, and hearing
- Coordination
- Balance
- Moodmemory
Lab examination
- Blood test- Blood may be collected from you for a variety of laboratory tests, such as those that look for antibodies frequently linked to paraneoplastic disorders. Additional tests might look for an infection, a hormonal issue, or a problem with how nutrients are processed (metabolic disease) that might be the source of your symptoms.
- Back tap (lumbar puncture)-Cerebrospinal fluid (CSF), the fluid that cushions your brain and spinal cord, can be sampled through a lumbar puncture. A small amount of CSF is extracted from your lower spine by a neurologist or properly trained nurse for laboratory testing.
While paraneoplastic antibodies cannot be recognised in your blood, they may occasionally be discovered in CSF. If these antibodies are discovered in both your blood and CSF, it is clear that a particular type of immune system activation is what is causing your nervous system symptoms.
Imaging exams
Imaging studies are utilised to locate a tumour that could be the root of your neurological problems or to find other causes. It's possible to use one or more of the following tests:
- Magnetic resonance imaging (MRI).
A magnetic field and radio waves are used in magnetic resonance imaging (MRI) to produce fine-grained cross-sectional or three-dimensional images of the tissue in your body.
- Positron emission tomography (PET) creates cross-sectional or three-dimensional images of the body. PET scans can be used to find malignancies, assess tissue metabolism, visualise blood flow, and find anomalies in the brain connected to seizures.
Combining PET with CT, or PET plus CT, may improve the likelihood of finding tiny tumours, which are frequent in persons with paraneoplastic neurological diseases.
The issue can still be caused by a tumour that is too small to be found, even if no malignant tumour is found or no other cause is found. The tumour may be triggering a strong immune response that is preventing it from growing much larger.
Management of PNS
While treating neurological paraneoplastic disorders, the immune response that is producing your symptoms and signs may also be suppressed in addition to the malignancy. The following choices may be part of your treatment, depending on the precise type of paraneoplastic syndrome you have:
Medications
Your doctor may give one or more of the following medications to prevent your immune system from attacking your nervous system in addition to treatments such as chemotherapy to treat your cancer:
- Prednisone is one example of a corticosteroid that reduces inflammation.
- Azathioprine (Imuran, Azasan), mycophenolate (CellCept), rituximab (Rituxan), and cyclophosphamide are among possible medications (Cytoxan).
Other drugs may include depending on the neurological illness and symptoms.
- Anti-seizure drugs could help manage seizures brought on by conditions that disrupt the electrical activity in the brain.
Drugs that increase nerve-to-muscle communication, which may alleviate the symptoms of disorders that compromise muscular function. A chemical messenger that carries a signal from nerve cells to muscles is enhanced by some medicines. The breakdown of these chemical messengers is prevented by other medications like pyridostigmine (Mestinon, Regonol).
- Plasmapheresis. Using a tool called a cell separator, this procedure separates your blood's fluid component, known as plasma, from your blood cells. Your platelets, white blood cells, and red blood cells are all returned to your body by the technicians, who also remove the plasma (which includes undesirable antibodies) and replace it with other fluids.
- Injectable immunoglobulin (IVIg). The healthy antibodies in immunoglobulin come from blood donors. High immunoglobulin levels hasten the breakdown of the harmful antibodies in your blood.
Additional treatments
If a paraneoplastic condition has resulted in a major handicap, other treatments might be beneficial:
- Physical treatment. You might be able to restore some lost muscle function with the aid of certain exercises.
- Speech treatment. A speech therapist can assist you in relearning the required muscle control if you are having difficulty swallowing or speaking.









