Some people may get viral or bacterial pneumonia. This suggests that airborne droplets can spread when inhaled from a cough or sneeze. Certain types of pneumonia can also be transmitted through contact with surfaces or objects...
Introduction
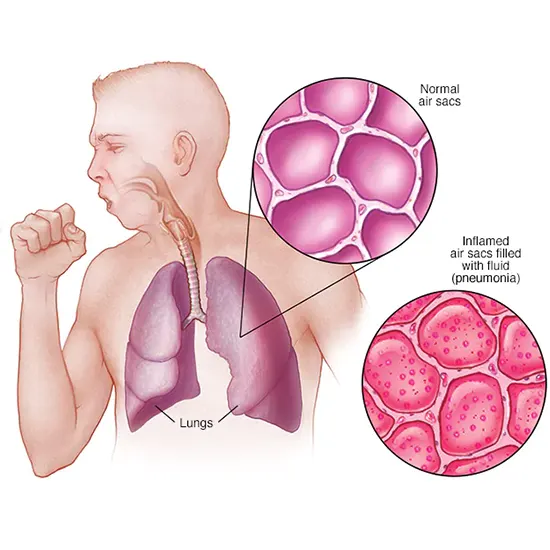
Infections known as pneumonia are caused by bacteria, or fungi. It causes inflammation in one or both air sacs of the lungs. When these sacs, called alveoli, fill with fluid or pus, breathing becomes difficult.
Some people may get viral or bacterial pneumonia. This suggests that airborne droplets can spread when inhaled from a cough or sneeze. Certain types of pneumonia can also be transmitted through contact with surfaces or objects that are contaminated with disease-causing bacteria.
Classification of Pneumonia
Pneumonia is further divided into the following categories based on where and how it was acquired:
- Hospital-acquired pneumonia (HAP) - This particular bacterial pneumonia develops while being treated in a hospital. This bacterium may be more harmful than other species because it can develop drug resistance.
- Community-acquired pneumonia (CAP) - This is pneumonia acquired outside a hospital or other institution.
- Ventilator-associated pneumonia (VAP) - Pneumonia in ventilator-dependent patients is referred to as VAP. Aspiration pneumonia is caused by inhaling bacteria into the lungs through food, drink, or saliva. It is more likely to occur if you are very sleepy after using tranquilizers.
Walking Pneumonia
Mild pneumonia is called migratory pneumonia. People suffering from mobile pneumonia may not even know they are ill. Unlike pneumonia, its symptoms may look like mild respiratory illness. However, ambulatory pneumonia may take longer to recover.
Symptoms of migratory pneumonia include:
- Light heat
- A prolonged dry cough of more than a weekCold
- Difficulty breathing
- Chest pain
- Loss of appetite
Bacteria and viruses, including Streptococcus pneumoniae, frequently cause pneumonia. and Haemophilus influenzae. However, Mycoplasma pneumoniae is a bacterium that typically causes migratory pneumonia.
Stages of Pneumonia
Pneumonia can be classified according to which part of the lung is affected:
- Bronchopneumonia - Both lungs can be affected by bronchopneumonia. It often occurs in or around the bronchi. A tube that connects the lungs and the trachea.
- Lobar pneumonia - Lobar pneumonia affects one or more lobes of the lung. Lobes are different regions of the lung that make up each lung.
Lobar pneumonia is further divided into 4 stages according to the course:
- Traffic jam
- Red hepatitis
- Gray liver
- Resolution
Cause
Pneumonia can be caused by many bacteria. Bacteria and viruses are most prevalent in the air we breathe. Normally, the body prevents harmful bacteria from entering the lungs. But even if your health is generally good, these viruses can overwhelm your immune system.
There are different types of pneumonia, depending on the type of pathogen and the mode of infection.
Community-Acquired Pneumonia
Pneumonia obtained in the community is the most typical type. It occurs outside a health care facility, such as a hospital. It can be caused by:
- Bacteria - Streptococcus pneumoniae is the leading cause of bacterial pneumonia in the United States. This type of pneumonia can develop on its own or after a cold or flu. Lobar pneumonia is a condition that can affect only her one lobe of the lung.
- Bacteria-Like Organisms - Mycoplasma pneumoniae can potentially cause pneumonia.Symptoms are usually milder than other pneumonias. This type of pneumonia is often not severe enough to require bed rest and is informally known as 'mobile pneumonia'.
- Fungi - People with weakened immune systems, chronic health problems, or people who have inhaled high levels of microbes are more likely to get this type of pneumonia. It can be found in soil or in bird droppings.
- Viruses, including COVID-19 pneumonia - can be caused by several viruses that cause colds and flu. Viruses are the most common cause of pneumonia in children under five. Ordinary viral pneumonia is not serious. But in some cases it can be very bad. Pneumonia caused by the 2019 coronavirus (COVID-19) can develop into serious cases.
Nosocomial Pneumonia
Some patients hospitalized with another illness develop pneumonia. Hospital-acquired pneumonia can be serious because the infected person is already sick and the bacteria that cause it may be more resistant to treatment. This type of pneumonia is common in intensive care units. More common in patients on mechanical ventilation.
Healthcare-Associated Pneumonia
Bacterial infections, known as “healthcare-associated pneumonia,” affect patients treated in outpatient clinics, such as dialysis facilities, or living in long-term care facilities. Hospital-acquired pneumonia can also be caused by bacteria that are more resistant to antibiotics than hospital-acquired pneumonia.
Aspiration Pneumonia
Aspiration pneumonia occurs when food, drink, vomit, or saliva is inhaled into the lungs. B. Brain injury, trouble swallowing, heavy alcohol or drug use, aspiration is likely when something interferes with your natural gag response.
Risk factors
Pneumonia can affect anyone. But her two age groups at highest risk are:
- Children under 2 years old
- Over 65 years old
- Other risk factors are:
Chronic disease -You are more prone to develop pneumonia if you have asthma, heart disease, or chronic obstructive pulmonary disease (COPD).
Smoking - The body's natural defences against the viruses and bacteria that cause pneumonia are weakened by smoking.
Weakened or suppressed - the immune system. HIV/AIDS patients who have received organ transplants, chemotherapy or long-term steroids are at risk.
Indication
Symptoms of pneumonia can range from mild to severe, depending on your age, general health, and the type of bacteria you are infected with. Mild symptoms and signs often resemble those of a cold or the flu, but last longer.
The following signs and symptoms of pneumonia may appear:
- Chest pain when coughing or breathing
- Confusion or altered consciousness (adults over age 65)
- Cough that can lead to phlegm
- Malaise
- high temperature, sweating, chills
- Lower-than-average body temperature (adults over 65 and people with weakened immune systems)
- Diarrhea, vomiting or nausea
- Difficulty breathing
Infants and newborns may not show symptoms of infection. Alternatively they might vomit, develop a fever or cough, appear drowsy, worn out, or under the weather, have trouble breathing, or have trouble eating.
Pathophysiology
Acute lung inflammation (pneumonia) brought on by an infection is referred to as pneumonia Infection with bacteria, mycobacteria, viruses, fungi, or parasites is possible. Healthcare professionals should remember that the term "pneumonia" actually refers to a series of syndromes caused by a variety of causes that lead to inflammation and sequelae.
The respiratory tract is commonly invaded by microorganisms, but many conditions prevent colonization.
- Slime blockage
- Cilia clearance
- Factors such as an intact epithelial barrier and immune surveillance
- Defensins and secreted IgA surfactant proteins (SP-a, SP-d)
- Pneumonia can result from the disruption or overwhelm of these defense mechanisms, allowing bacteria to colonize the lungs.
Nasopharyngeal secretions or other aspirated fluids can overwhelm upper airway defenses and cause infection. Inhaling the bacteria released into the air can spread diseases such as influenza and tuberculosis. Others are inserted into an endotracheal tube to bypass upper airway defenses.
Detection of infection by macrophages in the lower respiratory tract and alveoli elicits a strong immune and inflammatory response.
Lung consolidation results from an influx of inflammatory cytokines, leukocytes, and edema into the bronchi and alveoli.
A mismatch between ventilation and perfusion (V/Q) leads to hypoxemia. Infection can spread to other organs, the pleura, or the bloodstream (bacteremia and sepsis) (eg, meningitis).
The Four Stages of Pneumonia:
- Stage 1- Congestion is the early stage of pneumonia and usually occurs within the first 24 hours. Patients experience alveolar fluid, swollen blood vessels, and a variety of microbes. The lungs become very swollen and red. When the capillaries in the alveolar walls become blocked, the infection spreads to the pleura and hilum. During this stage, a person coughs and takes a deep breath.
- Stage 2 – After a few days of congestion, erythroid hepatitis develops. The lungs become purple like the liver, hard and airless. Vascular congestion persists, and the alveolar capillaries become swollen with blood. Alveoli fill with red blood cells, neutrophils, desquamated epithelial cells, and fibrin.
- Stage 3 – Gray hepatosis After 2-3 days after red hepatosis he has late sclerosis lasting 4-8 days. With hemosiderin, progressive erythrocyte degradation, and fibrinopurulent exudate, erythrocytes are degraded and appear gray with a liver-like consistency. Macrophages begin to appear.
- Stage 4-7 days, the lung structure begins to collapse and recover. Once solidified, the fibrous material is enzymatically liquefied and spread outward from the core, restoring ventilation. The majority of cells that carried debris and engulfed neutrophils are macrophages.
Diagnose
Doctors first take a medical history, do a physical examination, and use a stethoscope to listen for unusual bubbling or crackling sounds that may indicate pneumonia.
The following tests may be recommended by your doctor if pneumonia is suspected:
- Blood test - Blood tests are used to confirm infection and identify the specific type of organism that causes it. However, exact identification is usually not possible.
- Chest x-ray - This helps doctors diagnose pneumonia and determine the location and severity of the infection. However, you can't tell your doctor what type of organism is causing the pneumonia.
- Pulse Oximeter - It measures the amount of oxygen in the blood. Pneumonia can prevent the lungs from getting enough oxygen into the blood. Sputum examination. During a severe cough, a sample of fluid (sputum) from the lungs is taken and tested to determine the cause of the infection.
If you are over 65, are hospitalized, have severe symptoms, or have a medical condition, your doctor may order additional tests. They can consist of:
- CT scan - If pneumonia does not improve as expected, your doctor may recommend a chest CT scan to get a more accurate picture of your lungs.
- Pleural effusion analysis - A sample of fluid from the pleural area is taken by inserting a needle between the ribs and tested to determine the type of infection.
Prevention
- Update vaccination. All infants should start a series of vaccinations to protect against bacterial pneumonia starting at 2 months of age.
- All children over the age of 6 months should be vaccinated against the flu every year, even if they have an egg allergy.
- Instruct children to cover their mouth and nose with a shirt sleeve or handkerchief when they sneeze. Discard the tissue after use.
- Practice and teach proper hand washing.
- Frequently touched surfaces (toys, tables, doorknobs, etc.) should be cleaned with soap and water or a disinfectant.
- Continue smoking outside the home.
Treatment
The goal of pneumonia treatment is to eliminate infection and prevent consequences. The majority of the time, home medicine can be used to treat community-acquired pneumonia. Most symptoms go away in a few days or weeks, but fatigue can last him a month or more.
The type and severity of your pneumonia, your age, and your general health will all affect the specific treatment you receive.
- Antibiotics
- Cough syrup
- Antipyretic
- Pain reliever
Hospitalization
Hospitalization may be necessary if:
- You are over 65 years old. I don't know the dates, people, or places.
- Have decreased renal function
- Diastolic blood pressure is 60 mm Hg or less, or systolic blood pressure is less than 90 mm Hg.
- Rapid breathing (at least 30 breaths per minute)
- Need help breathing.
- Your body temperature is low
- Your heart rate is above or below 50.
If you need a ventilator or if your symptoms are severe, you may need to be admitted to an intensive care unit. A child may be hospitalized if:
- They are less than 2 months old.
- Appearing dehydrated, having trouble breathing, drowsy or lethargic. In addition, the blood oxygen level is low.
Prognosis
Pneumonia prognosis is influenced by a number of variables, including age, comorbidities, and hospital location (inpatient or outpatient). In general, prognosis is good in otherwise healthy patients. People under the age of 4 or over the age of 60 have a significantly worse prognosis than younger adults. If pneumonia is left untreated, all-cause mortality may rise to he 30%. Excessive and inappropriate use of antibiotics has caused a serious problem of antibiotic resistance. The Pneumonia Severity Index (PSI) can be used to calculate a patient's risk of death.
S. pneumoniae was identified as the cause of death in the majority of patients in CAP etiology studies. However, Pseudomonas, Staphylococcus aureus, and mixed etiology had the highest mortality among affected individuals.









