A disorder known as prostatitis causes inflammation of the prostate gland, a little gland found in the male reproductive system. The urethra, which transports urine and semen out of the body, is surrounded by the prostate...
What is Prostatitis?
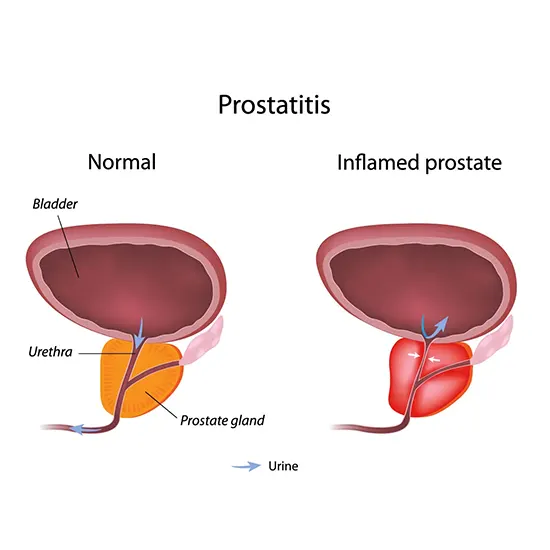
A disorder known as prostatitis causes inflammation of the prostate gland, a little gland found in the male reproductive system. The urethra, which transports urine and semen out of the body, is surrounded by the prostate gland, which also generates and stores fluid that constitutes a portion of semen.
Many symptoms, such as pain or discomfort in the pelvic area, trouble urinating, frequent urination, pain during ejaculation, and even flu-like symptoms like fever and chills, can be brought on by prostatitis.
The Prostate is What?
The prostate is a gland present in males. The fluid that becomes semen is mostly produced by the prostate. A man's prostate fluid must be present for him to be fruitful. The prostate is located in front of the rectum, underneath the bladder, and has two or more lobes, or parts, that are encircled by an outer layer of tissue.
How Widespread is Prostatitis?
Prostatitis symptoms are present in half of all men at some point in their lives. It is most common in men under the age of 50. It comes in third place among the factors that kill men over 50. More than two million men with prostatitis symptoms consult a doctor each year.
Is Prostate Cancer a Symptom of Prostatitis?
Prostatitis is not harmful (not cancerous). It doesn't make you more likely to develop prostate cancer. Yet, just like prostate cancer, prostatitis can occasionally cause inflammation that increases the blood level of prostate-specific antigens (PSA). Determine the cause of the elevated PSA levels with the use of additional testing.
Classification of Prostatitis
Prostatitis often comes in four different forms:
- Acute bacterial prostatitis: A UTI can infect the prostate gland, leading to acute bacterial prostatitis. Chills and fever are among the symptoms. You can have a difficult time peeing, have uncomfortable frequent urination, or both.
- Chronic bacterial prostatitis: Recurrent UTIs that are challenging to cure are brought on by bacteria that become lodged in the prostate gland.
- Chronic prostatitis or chronic pelvic pain syndrome: Continuous or recurrent pelvic pain and symptoms of the urinary system without signs of infection due to chronic prostatitis or chronic pelvic pain syndrome.
The most typical kind of prostatitis is called chronic pelvic pain syndrome, or CPPS. Prostate gland inflammation occurs in around 1 out of 3 males. As the name says, this variety produces persistent pain in the pelvis, perineum (the area between the scrotum and rectum), and genitals.
- Asymptomatic inflammatory prostatitis: It produces inflammation of the prostate gland but has no visible symptoms. You might find out you have this.
Symptoms of Prostatitis
Symptoms and symptoms of prostatitis might vary based on the type of disease.
They may consist of:
- During urinating, there may be pain or burning (dysuria)
- Urination difficulty, including dribble or hesitant urination
- Frequent urination, especially after dark (nocturia)
- Need to urinate immediately
- Foggy urine
- Urine with blood in it
- Abdominal, groin, or lower back pain
- Discomfort between the rectum and the scrotum
- Unpleasant ejaculation
- Other flu-like symptoms such as a fever, chills, and body aches (with acute bacterial prostatitis)
Acute Bacterial Prostatitis
Acute bacterial prostatitis is characterized by abrupt onset and severe symptoms. Males should get medical help right away.
Acute bacterial prostatitis symptoms may include the following:
- Urination routine
- A burning sensation or pain while urinating pain in the groin, lower abdomen, or lower back, as well as urinary urgency and fever chills
- Nocturia- regular nighttime urination
- Nausea and vomiting, bodily aches
- Having problems initiating a urine stream or having a weak or interrupted pee stream is known as urinary retention.
- As evidenced by germs and infection, urinary obstruction, or the total inability to urinate, is a sign of a UTI.
- Attacking cells present in the urine
Chronic Bacterial Prostatitis
Although less severe, the signs and symptoms of chronic bacterial prostatitis are comparable to those of acute bacterial prostatitis. This kind of prostatitis frequently takes time to develop and can persist for three months or longer. The symptoms could be intermittent or persistently mild. After earlier treatment for acute bacterial prostatitis or a UTI, chronic bacterial prostatitis may develop.
The signs and symptoms of long-term bacterial prostatitis include:
- Urination routine
- Urinary urgency a burning sensation or discomfort when urinating pain in the lower back, groin, abdomen, or genital region
- Unpleasant ejaculation
- Urinary obstruction, urinary retention, difficulty initiating a urine stream, a weak or intermittent urine stream, and a UTI.
Whenever to Visit a Doctor
The symptoms and signs of prostatitis can be caused by a variety of illnesses. The importance of receiving prompt diagnosis and care cannot be overstated.
If any of the following apply for emergency care:
- Being unable to urinate
- Fever and painful or difficulty urinating
- Urine with blood in it
- Extreme discomfort or pain in the genitalia or pelvic region
The Etiology of Prostatitis
- Acute bacterial prostatitis: Popular bacterial pathogens are generally to criticise for acute bacterial prostatitis. The spread of the virus may have originated in the urinary or reproductive systems.
- Chronic bacterial prostatitis: The aetiology of acute bacterial infection is typically the same as the cause of chronic bacterial prostatitis. It might happen when an acute illness isn't treated for long enough or doesn't completely eradicate the bacterium.
- Chronic prostatitis/chronic pelvic pain syndrome: It is unclear what causes chronic prostatitis/chronic pelvic discomfort syndrome. According to research, a variety of factors may interact. They include past infections, immune system or nervous system issues, stress-related issues, or abnormal hormone activity.
- Asymptomatic inflammatory prostatitis: Asymptomatic inflammatory prostatitis, which has no symptoms and no known aetiology, is typically only discovered during a medical examination for another condition.
Who is More Likely to Develop Prostatitis?
Prostatitis risk factors include:
- Young adulthood or middle age
- History of prostatitis
- HIV infection or AIDS infection of the reproductive or urinary systems
- Bladder drainage via catheter
- Prostate tissue sampled for diagnostic purposes (biopsy)
Other risk factors for chronic prostatitis and chronic pelvic pain syndrome include the following:
- Trauma or surgery-related tension pelvic nerve damage in mental health
Complications of prostatitis
Acute prostatitis may cause the following complications:
- Blood infection caused by bacteria (bacteremia)
- Infection of epididymitis
- Prostate cavity filled with faeces (prostatic abscess) Infection that spreads to the higher pelvic bone or lower spine
Complications of chronic prostatitis/chronic pelvic pain syndrome could include:
- Moodiness or worry
- One example of sexual dysfunction (erectile dysfunction) sperm and semen alterations that could cause infertility is the inability to get and maintain an erection.
Diagnosis of Prostatitis
There are numerous conditions that might result in the symptoms of prostatitis. An expert in problems of the urinary and reproductive systems may be recommended to you (urologist). Your doctor will perform a physical examination, go through your symptoms and medical history, and prescribe tests to pinpoint the problem's cause and rule out potential causes.
The following diagnostic tests will likely be performed to check for infection:
Digital Rectal Examination
A lubricated, gloved finger is inserted into your rectum during this operation to look for prostate inflammation.
a urine test. To check for the presence and type of bacterial infection, a urine sample will be required.
A Blood Test
For indications of infection and other prostate issues, blood samples may be examined.
Test on a Prostate Specimen
Occasionally, a doctor performing a rectal exam will gently massage your prostate to let any trapped prostate fluid flow into your urethra. After the massage, a urine sample is taken for bacterial testing, expelling the prostate.
Cystoscopy
During a cystoscopy procedure, the urethra and bladder are visualised inside a tube-like equipment called a cystoscope. The lower urinary system is entered by a urologist using the cystoscope through the hole at the tip of the penis. He or she does a cystoscopy in a hospital, an outpatient facility, or during a visit to the doctor's office. He or she will administer local anaesthetic to the patient. The patient could occasionally need sedation as well as regional or general anaesthesia. A urologist may employ cystoscopy to scan the urinary system for obstruction, narrowing, or stones.
Urinalysis
A urine sample is examined during a urine analysis. In a medical professional's office or another setting, the patient collects a urine sample in a particular container. The sample is examined by a doctor at an office visit or sent to a lab for examination. For the test, a nurse or technician puts a strip of chemically treated paper, called a dipstick, into the urine. When there is evidence of infection in the urine, patches on the dipstick change color.
The medical professional can identify the bacterial forms of prostatitis by using a microscope to examine the urine sample. In order to perform a culture on the sample, the healthcare provider may also submit it to a lab. A lab technician adds a few of the urine's components to a culture.
Imaging
Imaging studies may be requested to find prostate abnormalities, unusual growths, or other issues in the pelvic area that may be causing pain.
Biopsy
A little bit of prostate tissue is removed during a biopsy process to be examined under a microscope. The biopsy is carried out by a urologist in a hospital or an outpatient facility. He or she will administer a local anaesthetic and light sedation to the patient; however, in some circumstances, total anaesthesia may be necessary. The biopsy needle is guided into the prostate by the urologist using imaging methods including ultrasound, computed tomography, or magnetic resonance imaging. The prostate tissue is examined in a lab by a pathologist, a medical professional who focuses on analysing tissues to identify illnesses. The test can reveal the presence or absence of prostate cancer.
Treatment of Prostatitis
The type of prostatitis you have will determine how it is treated, as well as your symptoms.
Infection Treatment
Antibiotics are prescribed if you have either acute or persistent bacterial prostatitis. For a brief period of time in the hospital, intravenous (IV) antibiotics may be required for an acute disease. An antibiotic treatment course typically lasts 4 to 6 weeks, but it can occasionally go longer. It's critical to take all of the suggested medication in order to get rid of the infection and lower your risk of developing chronic bacterial prostatitis.
Treating Urination Issues
Alpha-blocker medications aid in relaxing the bladder neck and the muscle fibres where your prostate connects to your bladder. This treatment may help with bladder problems like difficult or unpleasant urination. Although this is frequently given for males with chronic prostatitis/chronic pelvic pain syndrome, it may also be used to treat bacterial infections' urinary symptoms.
Relieving Pain
By prescribing painkillers such as Advil, Motrin IB or acetaminophen (Tylenol, among others).
Taking Care of Psychiatric Symptoms
To assist you manage stress, depression, or anxiety that may be related to chronic pain, your doctor may advise psychotherapy with a mental health expert.
A Way of Life and DIY Remedies
Some symptoms of prostatitis may benefit from the following treatments:
- Warm bath
- Avoid drinking alcohol, using caffeine, and eating foods that are hot or acidic since they can irritate your bladder.
- Drink plenty of water. As a result, you'll urinate more frequently, which will help your bladder clear out microorganisms.
Substitute Medical Care
Alternative treatments that appear to be effective at easing prostatitis symptoms include:
Biofeedback
A biofeedback specialist will instruct you on how to control specific bodily responses and functions, such as relaxing your muscles.
Acupuncture
In specific locations on your body, very fine needles are inserted through your skin at varying depths as part of this pain control procedure.
Herbal Cures
According to certain studies, rye grass pollen extract (cernilton) may be able to reduce the discomfort brought on by chronic prostatitis or chronic pelvic pain syndrome. Several herbal treatments for the pain brought on by prostatitis lack sufficient evidence.
How Likely are Those Who Have Prostatitis to Recover?
Acute bacterial prostatitis is treatable with antibiotics. In between 30% and 60% of men, these drugs also reduce the symptoms of chronic bacterial prostatitis.
"Prostatitis doesn't discriminate, but you can fight back."









