A rare and potentially fatal condition known as psoas abscess is characterised by an accumulation of pus inside the psoas muscle. A sizable muscle, the psoas, extends from the lower spine through the pelvis and into the upper...
When your back pain isn't just back pain: Psoas Abscess
Introduction:
A rare and potentially fatal condition known as psoas abscess is characterised by an accumulation of pus inside the psoas muscle. A sizable muscle, the psoas, extends from the lower spine through the pelvis and into the upper thigh. Psoas abscesses can be caused by a variety of factors, including infection, trauma, and inflammatory conditions. Common symptoms include fever, pain in the lower back or abdomen, and difficulty walking.
What is Psoas Abscess?
Psoas abscess is commonly known as iliopsoas abscess. A localised collection of pus in the iliopsoas muscle compartment characterises this uncommon disease. Primary psoas abscess, which is brought on by the hematogenous or lymphatic dissemination of a pathogen, and secondary psoas abscess are the two types.
Infections of the gastrointestinal or musculoskeletal systems are the most frequent reasons for secondary psoas abscesses. S. aureus and E. coli are the most commonly isolated bacteria in infections, which are frequently monomicrobial. The majority of polymicrobial lesions have gastrointestinal origins. The most preferred diagnosis method is computed tomography. Following the acquisition of blood cultures and, if practical, abscess cultures, empiric antibiotic treatment should be started right away. In a nonseptic patient, a small (3.5 centimetre) abscess can be treated solely with antibiotics.
Larger or multiloculated abscesses should be surgically removed or drained under image supervision. Any type of psoas abscess should have the underlying reason examined and treated.
What is Psoas Muscle?
If you have queries about psoas Abscess, then it is essential to know about Psoas Muscle.
They connect to your femur after passing through your pelvic and your fifth lumbar vertebra, which is located between your 12th and fifth thoracic vertebrae. They are the sole muscles that attach your spine to your thighs, in actuality.
Your psoas muscles enable you to squat and bend your legs and hips towards your chest, such as when climbing steps. When you sprint or walk, they also assist in the propulsion of your leg forward.
When you stoop to gather something up off the floor, your psoas muscles flex your trunk forward. Additionally, they support your vertebrae and trunk while you're sitting or moving around.
Various Causes of Psoas Abscess
The psoas abscess can be encountered by you in the following ways:
A primary psoas abscess is brought on by the hematogenous or lymphatic dissemination of a pathogen from a far-off source.
- most frequently brought on by a particular pathogen
- Injuries to the psoas muscle, such as trauma or ischemia, raise the risk of infection.
- Greater prevalence in Asia and Africa
Psoas secondary cellulitis is caused by the pathogen's continuous spread from a nearby infectious centre.
The primary emphasis could be:
- IBD (particularly Crohn's disease), colitis, appendicitis, diverticulitis, and pancreatitis are gastrointestinal conditions.
- Musculoskeletal conditions include osteomyelitis, especially of the spine, Pott disease, paraspinal abscesses, septic arthritis, typically of the child's hip, and infections of prosthetic joints
- Genitourinary: for instance, cystitis and pyelonephritis
- Cardiovascular: such as contaminated aortic endograft, endocarditis, and infectious endocarditis
- After vascular surgery, arterial catheterization, spinal surgery, or urinary system instrumentation, for example.
Different main infectious foci are linked to various causative pathogens.
Risk factors:
- Immunodeficiency (e.g., diabetes mellitus, HIV)
- Use of intravenous drugs
- Trauma
- Responsible bacteria
- The majority of the time, primary and secondary psoas infections are monomicrobial.
- Compared to primary abscesses, secondary abscesses are more apt to be polymicrobial.
Features Seen in Patients Suffering from Psoas Abscess:
Various clinical features are:
- A painful walk
- a lower back ache (flank pain)
- Fever
Symptoms that are not particular include lower abdominal pain, fatigue, and weight loss.
At repose, the affected hip is externally rotated and flexed.
Pain is brought on by passive extension and/or internal movement of the injured hip.
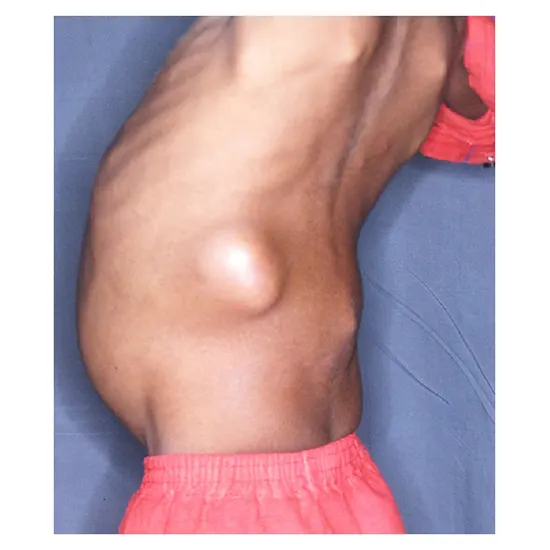
It's possible to feel a sensitive or non-tender mass in the ipsilateral inguinal or iliac area.
Additional characteristics: the presence of signs of underlying conditions (e.g., colitis, UTI).
Primary psoas abscess, which accounts for 30% of cases and is more prevalent in children, is caused by the hematogenous or lymphatic spread of infection from a distant occult site. Patients with immunocompromised conditions, like diabetes mellitus, are most likely to develop this condition. HIV/AIDS immunosuppressive medication drug use through injection kidney failure.
The majority of instances of secondary psoas abscess are caused by the direct growth of nearby inflammatory or infectious processes, which are most frequently linked to Crohn's disease.
Various gastrointestinal issues, such as diverticulitis, appendicitis, or colorectal cancer; genitourinary issues, such as urinary tract infections, cancer, extracorporeal shock wave lithotripsy, or instrumentation of the upper renal tract; and musculoskeletal issues, such as vertebral osteomyelitis, septic arthritis, or infectious sacroiliitis; are also linked to a secondary psoas abscess
How is the Diagnosis of Psoas Abscess Done?
However, abnormal findings may lead one to investigate infection as the source of the patient's symptoms. In general, laboratory testing is nonspecific in the diagnosis of psoas abscess.
- A complete blood count (CBC) Test and erythrocyte sedimentation rate (ESR) Test, C-reactive protein (CRP) Test, blood cultures, and urine (UA) may be ordered if the infection is suspected, including diskitis or psoas abscess.
- About 50% of individuals have positive blood cultures. ESR and CRP will typically be increased and could help track the progression of the anaemias. Anaemia and pyuria are also frequent.
- Because MRI appears to have no higher sensitivity or specificity than CT for diagnosing psoas abscess, and because ultrasound is only diagnostic in 60% of cases, IV contrast-enhanced spiral The imaging industry's ultimate standard is now CT.
- However, MRI offers a more thorough evaluation of all possible causes of back pain than CT because it is more effective at imaging the spinal canal.
- Additionally, a CT of the belly and pelvis with oral and intravenous contrast should be taken into account, particularly if another Psoas abscess is seen which is secondary.
- CT-guided drainage and fluid culture ultimately lead to a conclusive diagnosis and course of therapy.
Imaging:
Imaging is necessary to corroborate the clinical diagnosis of psoas abscess, according to the diagnosis. Laboratory tests offer corroborating proof of an acute contagious process and can be used to track treatment outcomes. The psoas abscess is assumed to be a primary psoas abscess if there is no readily apparent central focus of infection.
CT of the pelvis and abdomen with IV contrast (axial section) is recommended when:
- Typical discoveries
- Ipsilateral psoas muscle enlargement
- Encapsulated hypodense tumour with peripheral enhancement, with or without gas shadows, within the psoas muscle. This is a well-defined abscess.
MRI of the belly and pelvis with intravenous contrast.
Psoas cyst suspected in a patient with:
- The evaluation of back pain and suspected spinal pathology as contraindications for a CT scan, as well as the use of MR enterography in the case of Crohn's illness
- To be the main cause, it is thought. pregnant ladies should have MRIs without contrast.
- Distinctive results
- Abscess: T1 hyperintense, T2 hypointense
- Belly-scan ultrasound
A substitute for MRI in individuals who cannot undergo a CT scan. Ultrasonography of the abdomen:
Indications:
- In individuals who cannot undergo a CT scan, an alternative to MRI
- It is possible to use this imaging technique as the first line of defence in evaluating intraabdominal illness.
- Within the psoas muscle, the abscess shows as a hypoechoic collection.
Indications of pelvic or intra-abdominal :
- Imaging to assess a potential main focus
The diagnosis of a psoas abscess may unintentionally reveal a main focus in the spine or abdomen.
Keep in mind the following:
- Imaging to assess a potential main focus
- Having your main attention on your spine or belly
Think about the following:
- MRI scans of the spine are possible
spine-related osteomyelitis
- when there is a possible artificial joint infection, imaging of the hip or knee
Check out the differential diagnosis of low back discomfort as well.
- Digestive system
- Bowel inflammation, particularly
- Colitis
- Crohn's illness
- An appendicitis
- Pancreatitis and Diverticulitis
- Colorectal cancer
- Muscle and skeleton
- Bone inflammation (most commonly vertebral osteomyelitis)
- A paraspinal infection
- Hip-related septic arthritis (especially in children)
- Sciatica
- Muscle ache
- Idiopathic bursa
- A paraspinal infection
- Hip septic arthritis, particularly in children)
- Sciatic pain
- Muscle ache
Idiopathic bursa
- Iliopsoas muscle metastatic nodules
- Hip osteoarthritis.
- Hip prosthetic joint infection
- kidney pain
- Endometrial cancer
- An ectopic foetus that ruptured
- Cardiovascular
- Coronary malformation
- iliac artery endograft with infection
The collection of alternative diagnoses is not all-inclusive.
Drainage Techniques
Drain the abscess while using imaging guidance, then insert the drainage catheter into the abscess cavity to enable additional drainage. Drainage with CT guidance is recommended. You could try ultrasound-guided evacuation. If there are qualified doctors on hand.
Operative Draining
♦ Warning signs
Abscesses with multiple locations:
- Percutaneous drainage is unavailable for the abscess
- Sepsis or septic shock that is resistant to drug treatment
- The primary infection cause necessitates surgery
Checklist for acute care
If sepsis is prevalent, identify it and treat it.
- Before giving out antibiotics, obtain blood cultures and, if feasible, abscess fluid cultures.
- Treat psoas abscess with empiric antibiotic treatment.
- Speak with a surgeon and, if possible, a diagnostic radiography for draining an abscess.
- Offer comforting attention (e.g., analgesia, antiemetics, IV fluids)
- Think about patients' admittance to the ICU
How are Psoas Abscesses Handled?
- The preferred course of therapy for a psoas abscess entails both the drainage of the abscess and the administration of antibiotics.
- The pathogens implicated heavily influence antibiotic choice.
- To drain an abscess, a CT scan may be used percutaneously (through the epidermis) or during open surgery. Because it is minimally invasive, has a low risk of morbidity and mortality, and successfully treats almost all psoas abscesses, CT-assisted percutaneous drainage is the method of choice.
- Crohn's disease, diverticulitis, appendicitis, colorectal malignancy, urinary tract infection, vertebral osteomyelitis, mycotic abdominal aortic aneurysm, endocarditis, and history of instrumentation in or near the spine are all conditions linked to secondary psoas abscess.
Treatment options available for psoas Abscess:
The cornerstones of treatment are abscess drainage and antibiotic medication.
- When treating small abscesses (less than 3.5 centimetres), think about trying antibiotic therapy alone.
- Patients who are septic or if the abscess is big or multiloculated should have abscess drainage (either image-guided or surgical). Treatment with empiric antibiotics for psoas abscess
- Coverage: empiric treatment should spread of E. coli and S. aureus.
Recommended Diets
A beta-lactam with a beta-lactamase inhibitor from the following list:
- Ampicillin-sulbactam
- Piperacillin-tazobactam
- Metronidazole combination treatment
PLUS one of the subsequent
- a cephalosporin of the third generation, such as ceftriaxone
- A fluoroquinolone, such as levofloxacin PLUS, should be used to treat MRSA.
- Vancomycin
- Linezolid
When possible, adjust antibiotic therapy based on culture sensitivity reports.
As soon as the patient is afebrile, switch to oral medications.
Drainage of abscesses
Percutaneous discharge with images (PCD)
♦ Warning signs
- Abscess > 3.5 centimetres in size
- PCD is physically applicable to abscess
Keeping a Psoas Abscess from forming
Early diagnosis, prompt treatment, and elimination of complications before they develop can significantly reduce the risk of developing the disease.
When a patient has symptoms like fever, unbearable pain, pain with hip hyperextension, and psoas spasm, one should think about psoas abscess as a possible reason for their back pain. All psoas abscess patients need to be hospitalised for surgical or percutaneous drainage and antimicrobial therapy.
Psoas Abscess can be a rare but serious condition, don't underestimate its potential impact.









