In this article, we delve into the intricate realm of pulmonary hypertension, a complex and potentially life-threatening condition affecting the lungs and heart.
In this article, we delve into the intricate realm of pulmonary hypertension, a complex and potentially life-threatening condition affecting the lungs and heart.
We will explore its causes, symptoms, diagnosis, treatment options, and lifestyle considerations. By providing an in-depth understanding of pulmonary hypertension, we aim to empower individuals in their journey to combat this challenging disease.
Table of Contents:
- What is Pulmonary Hypertension?
- Causes and Risk Factors
- Recognizing the Symptoms
- Diagnostic Procedures
- Treatment Approaches
- Living with Pulmonary Hypertension
- Conclusion
What is Pulmonary Hypertension?
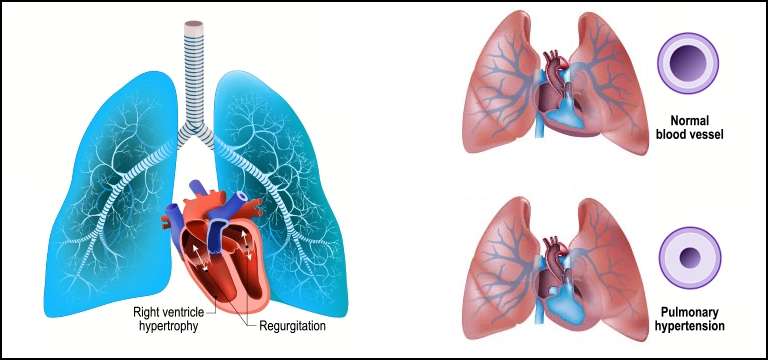
Pulmonary hypertension is a medical condition characterized by high blood pressure within the arteries of the lungs. This condition causes the heart to work harder to pump blood, leading to strain and potential damage to the heart and lungs over time.
Types of Pulmonary Hypertension
Pulmonary hypertension can be classified into different types based on its underlying causes and specific characteristics. Understanding these classifications is crucial for accurate diagnosis and appropriate treatment strategies.
Let's explore the main types of pulmonary hypertension:
Pulmonary Arterial Hypertension (PAH):
PAH is a primary form of pulmonary hypertension where the blood vessels in the lungs become narrow and thick, resulting in increased pressure. This type of pulmonary hypertension often lacks an identifiable cause, and it can be inherited or develop spontaneously.
Pulmonary Hypertension due to Left Heart Disease:
This type occurs when the left side of the heart is compromised, leading to increased pressure in the lungs. Conditions such as heart failure, valvular heart disease, or cardiomyopathy can contribute to this form of pulmonary hypertension.
Pulmonary Hypertension due to Lung Disease and/or Hypoxia:
Lung diseases, such as chronic obstructive pulmonary disease (COPD) or interstitial lung disease, can lead to pulmonary hypertension. Reduced oxygen levels in the blood (hypoxia) can also contribute to the development of this type.
Chronic Thromboembolic Pulmonary Hypertension (CTEPH):
CTEPH is a unique form of pulmonary hypertension caused by blood clots that obstruct the pulmonary arteries. These blood clots fail to dissolve naturally, leading to increased pressure and potentially life-threatening complications.
Pulmonary Hypertension with Unclear Multi-factorial Mechanisms:
Some cases of pulmonary hypertension do not fit precisely into any defined category. These cases often involve a combination of factors, including genetics, drugs, or other medical conditions.
Understanding the classification and types of pulmonary hypertension is crucial for accurate diagnosis, tailored treatment plans, and improved patient outcomes. By recognizing the specific characteristics and underlying causes, healthcare professionals can provide targeted interventions to manage this complex condition effectively.
Causes and Risk Factors of Pulmonary Hypertension
Pulmonary hypertension can stem from a diverse range of causes and risk factors, making it essential to explore the underlying triggers behind this complex condition.
While the exact mechanisms remain intricate and multifaceted, several key factors have been identified. Underlying medical conditions, such as congenital heart defects, connective tissue disorders, and chronic lung diseases, can contribute to the development of pulmonary hypertension.
Genetic predispositions, including inherited mutations in genes associated with pulmonary vascular function, can also play a role. Additionally, exposure to certain environmental factors like high altitudes or toxins can increase the risk of developing this condition.
Understanding these causes and risk factors is paramount for early detection, effective management, and improved outcomes for individuals affected by pulmonary hypertension.
Recognizing the Symptoms of Pulmonary Hypertension
Early recognition and prompt medical evaluation are crucial for timely intervention and improved management of pulmonary hypertension. Symptoms may initially be mild and easily dismissed, but as the condition progresses, they can become more pronounced and debilitating.
Following are the tell-tale symptoms of the disorder:
Shortness of breath, particularly during physical exertion or while lying down.
Fatigue and weakness, often accompanied by reduced stamina for daily activities.
Chest pain or pressure, which may worsen during exercise or exertion.
Rapid heartbeat or palpitations, indicating an increased workload on the heart.
Dizziness or fainting spells, potentially due to insufficient blood flow to the brain.
Bluish coloration of the lips, skin, or extremities (cyanosis), resulting from inadequate oxygenation.
Swelling in the ankles, legs, or abdomen due to fluid retention.
Dry cough or coughing up blood, indicating potential complications in the lungs.
Decreased appetite and unintentional weight loss, which can be symptoms of advanced stages of pulmonary hypertension.
Diagnostic Procedures of Pulmonary Hypertension
When it comes to diagnosing pulmonary hypertension, a comprehensive evaluation involving various diagnostic procedures is essential. Healthcare professionals employ a range of techniques to assess heart and lung function, measure pulmonary artery pressure, and identify potential underlying causes.
These may include physical examinations, medical history reviews, imaging tests such as echocardiograms and chest X-rays, and specialized procedures like cardiac catheterization.
Laboratory investigations, including blood tests and pulmonary function tests, are also crucial for confirming the diagnosis and ruling out other conditions.
By employing these diagnostic tools, healthcare providers can unravel the intricate nature of pulmonary hypertension, enabling tailored treatment plans and improved patient outcomes.
Treatment Approaches of Pulmonary Hypertension
Managing pulmonary hypertension requires a comprehensive and individualized treatment approach to alleviate symptoms, slow disease progression, and improve quality of life.
The treatment options for pulmonary hypertension encompass a range of strategies, including medication therapies, surgical interventions, and lifestyle modifications.
Medications and Therapies:
Vasodilators: Drugs like calcium channel blockers, prostacyclin analogs, and endothelin receptor antagonists help relax and widen the blood vessels, reducing pressure in the pulmonary arteries.
Anticoagulants: Blood-thinning medications can prevent the formation of blood clots that may worsen the condition.
Diuretics: These medications help manage fluid retention and reduce swelling.
Oxygen Therapy: Supplemental oxygen can improve oxygenation and ease breathing for individuals with low blood oxygen levels.
Clinical Trials: Participation in research studies and clinical trials can provide access to innovative therapies and potential breakthroughs.
Surgical Interventions:
Atrial Septostomy: In severe cases, creating a small hole between the upper chambers of the heart can relieve pressure and improve symptoms.
Lung Transplantation: For individuals with advanced pulmonary hypertension and significant lung damage, a lung transplant may be a viable option.
Lifestyle Modifications and Self-Care:
Regular Exercise: Engaging in supervised exercise programs tailored to individual needs can improve physical capacity and overall well-being.
Healthy Diet: A balanced diet rich in fruits, vegetables, lean proteins, and whole grains can support overall cardiovascular health.
Avoidance of Triggers: Minimizing exposure to environmental factors such as high altitudes, extreme temperatures, and certain medications or substances that can exacerbate symptoms.
Emotional Support: Seeking emotional support from counselors, support groups, and loved ones can help manage the psychological impact of living with pulmonary hypertension.
Collaboration between healthcare professionals, patients, and their support network is vital for optimal treatment outcomes. By combining medication therapies, surgical interventions when necessary, and adopting a healthy lifestyle, individuals with pulmonary hypertension can better manage their condition and lead fulfilling lives.
It is essential to work closely with medical providers to customize treatment plans and stay vigilant in the pursuit of managing this complex disease.
Living with Pulmonary Hypertension
Living with pulmonary hypertension presents unique challenges that require resilience, adaptability, and a supportive network. Individuals affected by this condition often face physical limitations and the need to make adjustments to their daily routines.
However, with the right strategies and a positive mindset, it is possible to maintain a fulfilling life. Emotional and mental well-being plays a crucial role, and seeking support from loved ones, support groups, or professional counselors can provide the necessary emotional support.
Managing daily activities involves pacing oneself, recognizing personal limitations, and prioritizing self-care.
Engaging in regular exercise programs tailored to individual needs, adopting a healthy diet, and adhering to treatment plans are integral components of maintaining overall health.
Awareness of available resources, such as educational materials and online communities, can provide valuable information and a sense of belonging.
By embracing resilience and nurturing life with pulmonary hypertension, individuals can thrive despite the challenges posed by this complex condition.
Conclusion:
Pulmonary hypertension poses formidable challenges, but with knowledge and a multidisciplinary approach, its impact can be mitigated. By raising awareness and promoting early detection, we hope to enhance the quality of life for those affected by this condition.
Remember, timely intervention, adherence to treatment plans, and a supportive network can make a significant difference in managing pulmonary hypertension.









