Actinomyces Israeli, A gerencseriae, and Propionibacterium propionicus (formerly Arachnida propionica) are the three pathogens that cause the typical actinomycosis in humans, a chronic disease.
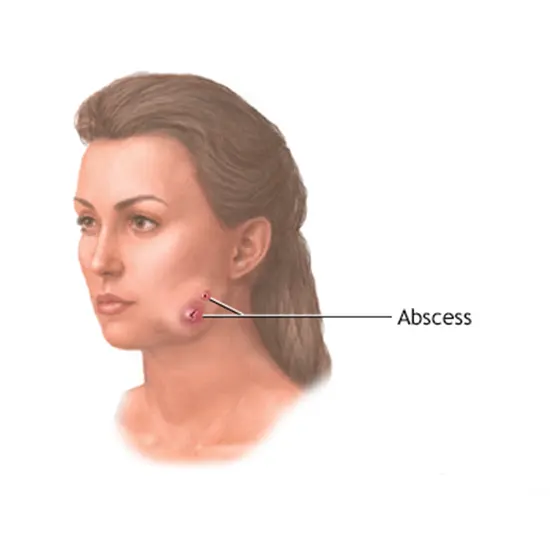
Actinomyces Israeli, A gerencseriae, and Propionibacterium propionicus (formerly Arachnida propionica) are the three pathogens that cause the typical actinomycosis in humans, a chronic disease. The infection is characterised by ongoing swelling, suppuration, and the development of abscesses with sinuses that are draining. The three main types are abdominal, thoracic, and cervicofacial. In addition to the bacteria that cause actinomycosis, several Actinomyces species have also been found in blood, the urinary system, eye infections, and other mixed anaerobic illnesses.
A broad number of pleomorphic Gram-positive bacteria, including Actinomyces species and Propionibacterium propionicus (formerly Arachnid propionica), exhibit a propensity for mycelial growth. Both are components of either the human or animal oral flora. Particular Actinomyces species are important contributors to tooth plaque. Actinomycosis in people and animals is brought on by the fungi A Israeli, A gerencseriae (formerly known as A Israeli serotype II), and P propionicus.
In mixed anaerobic and other infections, different Actinomyces species may be present but may not necessarily play a clearly pathogenic function. Additionally, novel species of Actinomyces have been discovered in several coryneform bacteria (diphtheroids) isolated from clinical samples and previously classified as Coryneform groups 1, 2, and E by the Centres for Disease Control.
Every organ is susceptible to actinomycosis. For instance, Actinomyces and P propionicus produce lacrimal canaliculitis with lingering concretions in the canaliculi. Eye infections are also possible with A naeslundi and A odontolyticus. Actinomyces and P propionicus have been isolated more frequently in recent years from female pelvic infections linked to the use of an intrauterine contraceptive device. Actinomyces' potential contribution to human periodontal disease and root surface caries has drawn a lot of attention. These bacteria do not appear to be responsible for the more severe types of periodontal disease, according to the available evidence.
Structure
Actinomyces, whose name translates to "ray fungus," are common microorganisms. Both Actinomyces and P propionicus are nonmotile, nonacid-fast, Gram-positive filamentous rods . Similar to other Gram-positive bacteria, muramic acid, N-acetylglucosamine, glutamic acid, and one or two other amino acids are present in the cell wall peptidoglycan.
The peptidoglycan of Actinomyces species comprises lysine or lysine plus ornithine, while P propionicus has L-diaminopimelic acid and glycine. A viscous and A naeslundii strains generally have well-developed long, thin surface fibrils. There are two types of pils (fimbriae) on A viscous and A naeslundii. Type 2 pili are involved in cloaggregation processes with other bacteria, whereas type 1 pili are involved in the adhesion of the bacteria to hard surfaces in the mouth.
Classification and Antigenic Types
The Gram-positive rods Actinomyces and P propionicum are asymmetrical and non-spore-forming. There are 19 species of Actinomyces and the two most prevalent human diseases are A Israeli and A gerencseriae. Chemotaxonomic assays, such as those on cell wall composition, fermentation products, and cellular fatty acids, DNA homology, and ribosomal RNA (rRNA) analysis, are used to define the genera Actinomyces and Propionibacterium. Some of the CDC Cornyeform groupings have been categorised as Actinomyces using these techniques.
On most rich culture media, Actinomyces and P propionicus grow successfully. They are best categorised as anaerobes that are aerotolerant. The species have different needs for oxygen. For example, A viscous and A naeslundii, an aerobic environment containing carbon dioxide is optimum for growth, but A Israeli needs anaerobic circumstances. Actinomyces and P propionicus both use the fermentation of carbohydrates to provide energy. Acetic, lactic, formic, and succinic acids are the primary byproducts of Actinomyces' fermentation of glucose, whereas Propionibacterium mostly produces propionic, acetic, and formic acids with a minor amount of succinic acid.
Actinomyces strains have recently been classified based on their DNA fingerprints in an effort to demonstrate the transmission of particular oral strains among individuals. Additionally, by recognising rRNA gene sequences in the DNA fingerprint, bacteria have been ribotyped. Oral A naeslundi i strain ribotyping has revealed that a person can have up to 5 ribotypes and that it is unusual for people to share ribotypes. These more recent techniques for genetic typing are probably going to help us learn more about the biology of Actinomyces, their epidemiology, and their connection to disease.
Pathogenesis
When oral bacteria that live in the mouth are transferred into the tissues, actinomycosis develops. There is no consensus on how Actinomyces and P propionicum cause illness. These organisms' capacity to inhibit some of the host's immune system processes may play a role in pathogenesis. Actinomyces is chemotactic, stimulates the release of lysosomal enzymes from polymorphonuclear leukocytes and macrophages, and activates lymphocyte blastogenesis, according to studies on oral illness.
Actinomyces and P propionicus do not produce considerable amounts of exotoxins or other poisonous compounds, with the exception of A pyogenes, which produces a hemolysin that is neutralised by antiserum and a soluble toxin. The development of abscesses and tissue invasion-promoting factors have not been proven.
Host Defences
Some healthy people, people with gingivitis and periodontitis, as well as people who have clinical actinomycosis, all circulate Actinomyces antibodies. This humorous reaction most likely doesn't contribute significantly to actinomycosis defence. Actinomyces and P propionicus, like other anaerobes in the normal flora, must enter tissue with a compromised blood supply in order to create an infection, making an intact mucosa the first line of defence. The host's cell-mediated immune response may limit the scope of the infection once the organisms have entered the tissues, but it may also cause tissue damage.
Epidemiology
In the absence of clinical disease, Actinomyces Israeli, A gerencseriae, A Georgian, A naeslundii, A odontolyticus, A Meyer, potentially A pyogenes, and P propionicus are common occupants of the tonsils, saliva, the tongue, and gingival crevice debris in the human mouth. According to some evidence, A Israeli may also frequently occupy the female vaginal tract.
Worldwide, actinomycosis is a problem. The condition affects men more frequently than women, but there is no correlation between race, age, or career. There is no proof to support the transmission of Actinomyces from person to person or from animal to human, with the exception of bite wounds on humans. The more recently identified Actinomyces may infect compromised patients.
Diagnosis
To look at the overall health doctor recommends tests such as CBC, CRP, PAP test to detect the changes in the body
The existence of granules in the specimens is initially checked. If present, the granules are crushed, stained with Gram, and checked for rods or branching filaments that are Gram-positive. A rich medium, such as brain heart infusion blood agar, is used to cultivate washed, crushed granules or well-mixed pus in the absence of granules. Carbon dioxide is supplied during anaerobic and aerobic incubation.
The typical colonies of A Israeli, A gerencseriae, and P propionicus, which resemble those of A Israeli, are looked for on plates after 24 hours and after 5 to 7 days . Other Actinomyces species' colonies can have a range of shapes, including flat or smooth-domed colonies of different sizes.
Immunofluorescence tests are helpful for the direct visualisation of the organisms in clinical samples as well as the serologic identification of isolates.
Because this bacterial infection affects the respiratory health, so to know about the health of your chest organs, doctor recommends Chest X-Ray and CT Scan Chest or MRI of chest.
Disease management
Actinomycosis requires long-term antibiotic therapy together with surgical drainage of the lesions and excision of injured tissue due to the mixed nature of the infection and the presence of granules (see above). Actinomyces species and P propionicus are susceptible to a wide range of antibiotics, including penicillins, cephalosporins, tetracyclines, chloramphenicol, and others. All Actinomyces species can be treated with penicillin; there is no known major antibiotic resistance.