The gram-negative, obligate intracellular bacterium Rickettsia prowazekii is what causes epidemic typhus, a serious illness that can be fatal. It is named for its discoverer, the pathologist Stanislaus von Prowazek, who was...
The gram-negative, obligate intracellular bacterium Rickettsia prowazekii is what causes epidemic typhus, a serious illness that can be fatal. It is named for its discoverer, the pathologist Stanislaus von Prowazek, who was born in the Czech Republic and recognized it in 1916.
Humans contract R. prowazekii from infected lice, primarily the human body louse, which is frequently present in crowded and unhygienic living situations. Once within the host, the bacterium enters KFT and multiplies within endothelial cells, resulting in a systemic infection that may cause symptoms including fever, headache, rash, and others. Typhus fever can develop into more serious complications, such as shock, organ failure, and even death if it is not promptly treated.
Even while epidemic typhus is now relatively uncommon in affluent nations, it nevertheless poses a serious threat to public health in places with subpar sanitation and hygiene, like refugee camps and conflict zones. Due to its high infectiousness, low infectious dose, and potential for aerosol transmission, R. prowazekii is also regarded as a potential biological weapon.
The Genetic Roadmap To Combating Rickettsia prowazekii.
When compared to other bacterial pathogens, Rickettsia prowazekii's genome, which is roughly 1.1 million base pairs in size, is comparatively tiny and compact. About 834 protein-coding genes make up the circular genome, which is a small number when compared to the genomes of other bacterial species.
It's interesting to note that R. prowazekii has undergone a process known as genome reduction, which has resulted in the loss of numerous genes and pathways that are not necessary for survival and replication within host cells. The adaptation of R. prowazekii to its intracellular lifestyle, in which it depends on host cells for many of its metabolic and biosynthetic processes, is thought to be the cause of this process of genome reduction.
Despite having a small genome, R. prowazekii has many genes involved in pathogenicity and virulence, such as genes that code for cell surface proteins, toxins, and other virulence factors. R. prowazekii also possesses several genes involved in DNA replication and repair as well as stress response pathways, all of which are crucial for the organism's survival inside host cells.
R. prowazekii exhibits a high level of genetic diversity, according to genomic studies, with strains isolated from various geographical locations displaying variations in their genomes. The development of potent typhus vaccines and therapies will be significantly impacted by this genetic variation.
The Life And Times Of Rickettsia prowazekii: A Journey Through Host Cells.
Humans contract Rickettsia prowazekii when an infected louse, often the human body louse, bites them (Pediculus humanus corporis).
The bacterium enters the blood vessel lining cells and starts a quick replication process.
R. prowazekii injects effector proteins into the host cell using a type IV secretion system. These effector proteins change the host cell signaling pathways, allowing the bacteria to evade the host's defenses.
The bacterium exploits the host's nutrition and cellular machinery for its growth and survival.
R. prowazekii makes outer membrane proteins that enable it to evade immune system recognition.
The bacterium can harm the endothelium and result in the development of distinctive skin lesions known as eschars.
The bacterium can cause systemic symptoms including fever, headaches, and muscle soreness by spreading to other organs and tissues.
The bacterium can eventually be returned to the arthropod carrier through the louse's excrement after several days.
During this time, if the louse feeds on another human host, the bacterium may spread through cracks in the skin or mucous membranes to the new host.
To create effective preventative and control measures for epidemic typhus, it is imperative to have a better understanding of the Rickettsia prowazekii life cycle, which includes various stages of development, replication, and transmission.
Bite-sized Danger: How The Human Body Louse Spreads Rickettsia prowazekii.
Humans are typically exposed to Rickettsia prowazekii through the bite of an infected human body louse (Pediculus humanus corporis). Contact with contaminated bedding, clothing, or other personal things of an infected person can also spread the bacteria.
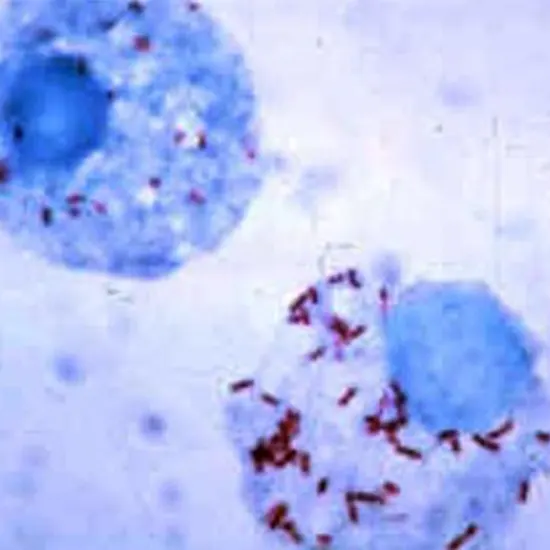
When a louse feeds on the blood of an animal or human with R. prowazekii infection, the cycle of transmission giemsa stain begins. The bacterium can be found in the lice feces, which can contaminate the skin around the bite wound or neighboring skin, as well as the mucous membranes.
Scratching the bite site can transmit the germs to other parts of the body by allowing them to enter the bloodstream through the skin.
R. prowazekii does not spread from person to person, but close contact with an infected person or their possessions can help the bacterium spread to healthy people.
Since lice infestations are more likely to happen in crowded, unsanitary settings, poor sanitation, and hygiene are strongly associated with the transmission of R. prowazekii.
Measures to reduce or eliminate lice infestations as well as to improve sanitation and hygiene are typically taken to prevent and control the spread of R. prowazekii. This can involve regular bathing, washing of clothing and bedding, the use of pesticides or other medications to treat lice infestations and instruction regarding the value of good hygiene and cleanliness.
What Can Be the Signs And Symptoms?
The bacteria Rickettsia prowazekii is responsible for the dangerous condition known as epidemic typhus. Upon exposure to the bacteria, this disease's signs and symptoms often start to manifest one to two weeks later and may include:
High fever: A high temperature, which can range from 102°F to 104°F (38.9°C to 40°C) and last up to two weeks, is the most typical sign of epidemic typhus.
Rash: A rash frequently starts on the body's trunk and moves to the arms and legs. The rash typically begins as little red dots and evolves to bigger, uncomfortable, and itchy purple areas.
Headache: Severe headaches from epidemic typhus can be incapacitating and chronic.
Muscle pain: The illness can lead to muscle pain, especially in the legs and back.
Sweating excessively: Patients with epidemic typhus may have profuse perspiration and chills, especially when they are experiencing fever.
Vomiting and nausea: Some patients may develop diarrhea, vomiting, and nausea.
Delirium: In severe circumstances, patients may go into a coma or experience bewilderment.
Diagnosing Rickettsia prowazekii: A Crucial Step In Controlling Spread Of Epidemic Thymus.
Diagnostic criteria for epidemic typhus, commonly known as Rickettsia prowazekii infection, combine clinical symptoms and laboratory findings. In regions where the disease is endemic, cect chest diagnosis can be difficult and may need a high level of suspicion due to the vague symptoms of epidemic typhus.
Clinical presentation: Although the severity of the symptoms might vary, sudden onset high fever, headache, muscle pains, and malaise are frequently present in epidemic typhus. After 5–6 days of fever, a distinctive rash that commonly begins on the trunk and progresses to the extremities may appear. In severe situations, problems like meningitis, renal failure, and pneumonia might happen.
Testing in the lab: Testing in the lab can help with the diagnosis of R. prowazekii infection. R. prowazekii DNA can be detected in blood samples cbc using polymerase chain reaction (PCR) assays, and specific antibodies to the bacterium can be detected in blood samples using serological tests like indirect immunofluorescence assay (IFA) or enzyme-linked immunosorbent assay (ELISA).
Further laboratory tests may be carried out in cases when the diagnosis is unsure to rule out other infectious disorders with comparable symptoms. Infections caused by other Rickettsia species, chest x-ray such as Rickettsia typhi or Rickettsia rickettsii, as well as other bacterial, viral, and parasite illnesses, may also be detected by these tests.
What Can Be Treatment Options?
Antibiotics: Tetracycline or doxycycline are the antibiotics of choice when treating epidemic typhus. In some circumstances, chloramphenicol or azithromycin may also be utilized.
Treatment time: Antibiotics are typically administered for a minimum of 7 to 10 days, but they may occasionally be prolonged for up to 21 days.
Supporting care: Patients with epidemic typhus may require supportive care, including intravenous fluids to keep their electrolyte levels balanced and hydrated, as well as drugs to reduce their fever and pain.
Hospitalization: Hospitalization may be necessary for patients with severe symptoms such as confusion, delirium, or respiratory distress.
Prevention: As infected body lice are the main means of spreading epidemic typhus, precautions should be taken to minimize exposure to them. This entails employing appropriate hygiene practices, protecting yourself from insects, and avoiding close contact with others who are ill.
It's important to remember that fast diagnosis and treatment are essential for a successful outcome. It's critical to get medical assistance right away if you think you could have epidemic typhus or that someone you know might.









