Ingesting various foods, especially processed meat and dairy products, that have been contaminated with S. aureus due to inappropriate handling and subsequent storage at high temperatures are the usual causes of food...
Ingesting various foods, especially processed meat and dairy products, that have been contaminated with S. aureus due to inappropriate handling and subsequent storage at high temperatures are the usual causes of food poisoning, which is a primary cause of SEs. Rapidly appearing symptoms include nausea and intense vomiting, together with or without diarrhoea. The sickness rarely becomes serious enough to necessitate hospitalisation and is typically self-limiting.
Although SEA is the most typical SE to induce staphylococcal food poisoning globally, other traditional SEs have also been shown to be involved. Only SEH has been clearly linked to food poisoning among the novel SE/SEls.
When foods contain enough of one (or more) preformed enterotoxins, it can cause staphylococcal food poisoning (SFP), which is an intoxication [1,2]. SFP symptoms include nausea, severe vomiting, abdominal cramping, and diarrhoea or other gastrointestinal distress.
These symptoms typically appear quickly (2–8 hours). The illness normally has a 24-48 hour latency period before clearing up on its own. Sometimes it can be severe enough to necessitate hospitalisation, particularly when newborns, the elderly, or persons with disabilities are involved.
Etiology
The primary cause of food contamination through manual touch or respiratory secretions is believed to be food handlers who have enterotoxin-producing S. aureus in their noses or on their hands. S. aureus is a typical commensal that lives on human skin and mucous membranes.
Meat and meat items, poultry and egg products, milk and dairy products, salads, bakery goods, especially pastries and cakes with cream fillings, and sandwich fillings are a few foods that have frequently been linked to staphylococcal poisoning. According to the ability of S. aureus to grow at relatively low water activity (aw = 0.86) salted food products, such as gammon, have also been implicated.
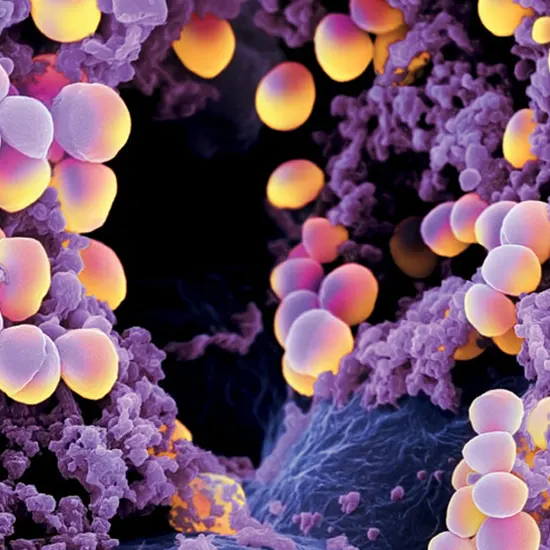
Structure and toxins
Toxins
The S. aureus enterotoxins (SEs) are strong gastrointestinal exotoxins produced by S. aureus during the logarithmic phase of growth or when the exponential phase changes to the stationary phase.
They are active in concentrations ranging from high nanogram to low micrograms, and they are resistant to circumstances (heat treatment, low pH, and proteolytic enzymes) that easily kill the bacteria CECT Whole Abdomen that make them. As a result, they continue to function in the digestive system after consumption.
Structures
SEs are a member of the superfamily of pyrogenic toxin antigens. By interacting with T-cell receptors (TCR) on particular T-cell subsets and major histocompatibility complex (MHC) class II molecules on the surface of antigen-presenting cells, SAgs avoid conventional antigen recognition.
Although binding to the TCR V domain has been documented, interaction often occurs to the variable portion of the TCR chain (V).This causes a huge number of T cells to become activated, which causes them to multiply and Ultrasound release enormous amounts of chemokine and pro inflammatory cytokines, which may cause toxic shock syndrome, a potentially fatal condition.
Mode of action
Although significant efforts have been made to pinpoint individual amino acids and SE domains that may be crucial for emesis, the available data is still few and debatable. Similar to TSST-1, SElL BUN Creatinine Ratio and SElQ are non-emetic, while SEI has sporadic emetic activity.These poisons lack the disulfide loop that is typically seen at the head of the N-terminal domain of other SEs.
The loop may stabilise a key conformation that is essential for this function, but it does not appear to be a necessary component of emesis. Histidines on SEA or SEB undergo carboxymethylation to produce proteins free of enterotoxicity while retaining their superantigenicity.
The effects of carboxymethylating each of the SEA histidines were examined, and it was discovered that His61 is crucial for emesis but not for T-cell proliferation.Emesis and superantigenicity are thus distinguished as distinct functions of the proteins by the fact that the mutant variants of SEA and SEB, Serum Electrolytes Leu48Gly and Phe44Ser, respectively, do not bind MHC class II molecules or activate T cells yet nevertheless cause vomiting.
Despite this, there is a strong association between the two behaviours because most of the time, genetic changes that cause a loss of super-antigen activity also cause a loss of emetic activity.
Enterotoxins and food poisoning
Regardless of where they came from, enterotoxigenic S. aureus frequently varies in the quantity of mobile genetic elements and se/sel genes they contain as well as the enterotoxins they Culture and Sensitivity produce. Because of its incredibly high resistance to proteolytic enzymes, SEA is the enterotoxin most frequently observed in foods, either alone or in combination with other SEs/SEls. It is also thought to be the primary cause of SFP.
In numerous nations, the prevalence of SEA has been well-documented. Relevant instances include:
A thorough analysis of 359 outbreaks that occurred in the United Kingdom (UK) between 1969 and 1990 found that 79% of the S. aureus strains produced SEA [121]. In 75% of the cases, gammon and chicken were the primary ingredients in the meat, poultry and goods they produce.
SEA was the enterotoxin most frequently found among 31 SFP outbreaks in France (69.7%), which were linked to a wide variety of foods including milk products, various types of meat, and salads. SEA was CBC detected alone in 56.9% of the outbreaks and in conjunction with SED, SEB, SEC, or SEB and SED in a lower number of outbreaks.
A study of S. aureus isolated from dairy products, responsible for 16 outbreaks in Brazil, revealed that the most commonly encountered enterotoxin gene was sea followed by seb. SEA was also the most common enterotoxin Stool Culture recovered from food poisoning outbreaks in the USA (77.8% of all outbreaks), followed by SED and SEB .
The world's SFP outbreaks have also been linked to SEB, SEC, or SED on their own. Interestingly, a community-acquired methicillin resistant S. aureus from an asymptomatic food handler produced coleslaw-containing SEC that led to an outbreak that sickened three members of the Gram Stain same family in the USA. SEE, the fifth classical enterotoxin, is rarely found in foods and animals that produce food, and its connection to SFP outbreaks has only occasionally been established.
But six SFP outbreaks that happened in France at the end of 2009 were brought on by SEE found in soft cheese prepared from raw milk. Additionally connected to outbreaks in the USA and the UK is this enterotoxin.
Conclusion
The SEs and SEls that S. aureus produces are interesting super-antigens that attack the host's innate and adaptive defences in an effort to compromise the immune system. When it comes to super-antigenic action, family members are well characterised.
The mechanisms underlying a number of S. aureus superantigens' enterotoxigenic activities, however, are yet unknown. S. aureus SEs, which have been shown to have emetic activity, and SEls, which do not have emetic activity or have not yet been tested, have not always been directly linked to pathogenicity, and the causes of the redundant se/sel genes within the same bacterium need to be further explored.
In particular, the egc cluster is intriguing since it is thought to be a nursery for se/sel genes that are still undergoing evolution.
There have been few attempts to clarify the pathogenic role of vgc-encoded SEs, and no evidence has been provided that they are directly responsible for food poisoning.
As a whole, SEs and SEls constitute an active area of research, and although though a plethora of information about them is already available, new and fascinating discoveries will undoubtedly be made in the years to come.









