In this blog, we will discuss about the GERD disease in detail.
What is Acid Reflux?
Acid reflux is the flow of acid backwards from your stomach to the Oesophageal region.
Acid irritates and inflames the tissues inside your oesophagus when it creeps to the places it does not belong, which may run from your stomach to your chest to your throat.
Symptoms of Acid Reflux
- indigestion,
- burning stomach pain after eating
- heartburn
- burning chest pain
Acid reflux is usually not a disease, but it can affect your quality of life and cause real damage to your tissues.
What is GERD?
GERD in medical terms means gastroesophageal reflux disease in your oesophagus. It is considered chronic if lasts for a few weeks.
This condition is temporary But GERD is a constant, mechanical problem. It means that the mechanisms that are supposed to keep acid out of your oesophagus aren’t working right.
How Common Are Acid Reflux and Gerd?
GERD is estimated to affect about 20% of adults and 10% of children in the U.S.
What Are the Symptoms of Acid Reflux and Gerd?
Its Symptom includes
- The backwash of stomach acid: You might observe that the food you eat backwash from the stomach to your throat also called regurgitation. You might notice the sour taste of the acid.
- A burning sensation: Excessive acid can lead to Acid burns in your oesophagus which may feel in the chest called heartburn.
- Chest pain: Due to excessive acid in the Esophagal region it can trigger the same nerves as heart-related pain
- Nausea: Acid reflux can cause soreness in the throat and mouth leading to loss of appetite and a feeling of Nausea that lasts for some time
- Sore throat: If acid rises in your stomach, it can make it sore throat making food hard to swallow Reflux into your throat often happens at night.
GERD symptoms may be worse if
- At night or while lying down.
- After heavy or fatty meals.
- After smoking or drinking alcohol.
What Causes Acid Reflux?
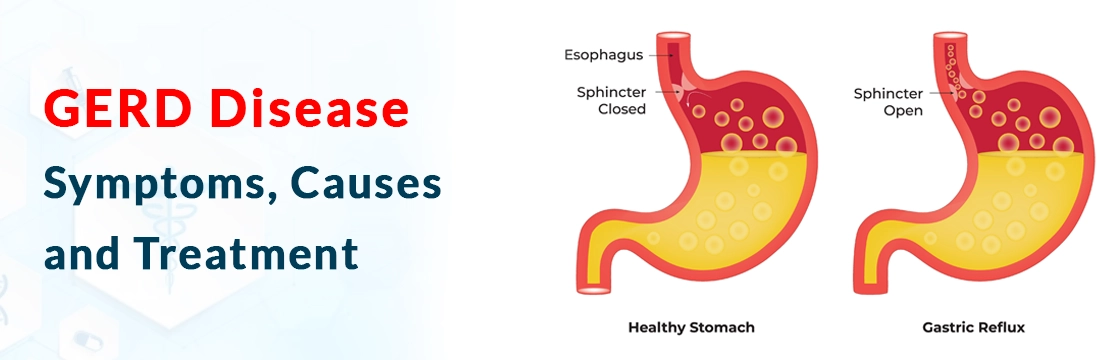
Acid reflux happens when your LES( lower oesophagal sphincter) weakens or relaxes enough to let acid pass. Some temporary things can relax your LES, like lying down after a large meal. But if you have GERD, it means your LES is relaxing often.
Many things can contribute to weakening your LES, either temporarily or permanently. Sometimes occasional acid reflux turns into chronic GERD when these factors overlap or persist for a long time.
Common causes of acid reflux and GERD include:
- Hiatal hernia: A Hiatal hernia is a very common hiatal hernia that happens when the top of your stomach pushes up through the hole in your diaphragm where your oesophagus passes through it generally occurs when you grow older and may gradually worsen if untreated.
- Obesity: When you gain excess weight it affects your LES similarly to how pregnancy does. That can weaken the muscles more permanently. And act as a contributing factor for hiatal hernia.
- Smoking: Smoking also relaxes your LES and also triggers coughing, which opens your LES. Smoking also affects your lungs and diaphragm muscles and also contributes to developing a hiatal hernia. Excess Smoking can lead to the formation of acid leads to GERD.
- Pregnancy: Temporary acid reflux is generally observed during pregnancy. Pregnancy hormones encourage your LES to relax. Pregnancy brings high levels of the hormone relaxin, which relaxes your muscles so they can stretch to make room for the fetus.
Other possible causes of GERD include:
Birth defects: These include Congenital defects like oesophagal atresia and hernias that can affect your LES.
Connective tissue diseases like scleroderma may affect your oesophagus muscles.
Medications
Certain medications can have a relaxing effect on your LES, including:
- Benzodiazepines, a type of sedative.
- Calcium channel blockers, which treat high blood pressure.
- NSAIDs (nonsteroidal anti-inflammatory drugs) like aspirin and ibuprofen.
- Theophylline is a common asthma medication.
- Hormone therapy (HT) medications for menopause
- Tricyclic antidepressants
Diagnosis and Tests
How is GERD Diagnosed?
A gastroenterologist will evaluate your oesophagus to diagnose GERD. Tests may include:
- Esophagram(X-ray): It is an X-ray examination that involves X-rays (fluoroscopy) of your oesophagus while you swallow. a chalky liquid called barium is swallowed during the procedure
- Upper endoscopy: It involves moving the camera in the Oesophageal region on the end of a thin tube that passes through your mouth while you’re asleep under light sedation.
- Oesophageal pH test: This test measures the acid content inside your oesophagus through a small wireless receiver.to measure the acidity level
- Oesophageal manometry: This test measures the muscle activity in your oesophagus to check for the Lower Oesphagal Sphinctor or other muscles that aren’t working right.
Management and Treatment
What is the medical treatment for GERD?
Some people find they can reduce acid reflux with lifestyle adjustments, like changing their eating habits, reducing alcohol and tobacco and losing weight. Healthcare providers encourage this approach.
But if you have chronic acid reflux or GERD, they also recommend medicines to reduce your stomach acid, so reflux is less damaging. These medicines are easily available and highly effective for GERD.
Medicine
Over-the-counter (OTC) medicines for acid reflux include:
- Antacids: They neutralize your stomach acid so that when reflux happens, it isn’t as corrosive to your oesophagus. They work well for occasional acid reflux.
- Alginates: Alginates are naturally occurring sugars derived from seaweed. They help block acid reflux by floating on top of the acid, creating a physical barrier between the acid and your oesophagus.
Prescribed medications for GERD include:
- Histamine receptor antagonists (H2 blockers): H2 blockers reduce stomach acid by blocking the chemical that tells your body to produce it (histamine).
- Proton pump inhibitors (PPIs): PPIs are stronger acid blockers that also promote healing. Your provider may prescribe them as a first-line treatment if your GERD is relatively severe or you have signs of tissue damage in your oesophagus.
- Baclofen: Baclofen is a muscle relaxant, often prescribed to reduce muscle spasms. It can also help reduce the frequency of LES relaxation events, and it also helps reduce acid reflux.
How Can I Reduce Acid Reflux at Home?
To help manage acid reflux at home, try:
- Eating smaller meals: Heavy meals lead to excess acid release while Smaller meals digest faster and don’t stimulate your stomach to produce so much acid.
- Eating dinner earlier: Eating dinner idea to eat several hours before reclining in the living room or going to bed
- Sleeping on your left side: This positions your lower oesophagal sphincter in an air pocket above your stomach contents and eases digestion.
- Stopping smoking and drinking: Both tobacco and alcohol weaken your LES. and increase acidity in the stomach, So avoid this completely.
- Over-the-counter medications.: Antacids and alginates are good to have on hand, especially if you know you’re eating a rich or acidic meal that might trigger more stomach acid.
A Note From Ganesh Diagnostic
Heartburn, indigestion and acid regurgitation become common if your eating habits are not good these problems can further worsen if not taken into account but you can take certain steps to reduce the frequency of these events.
For people with acid reflux, and if it becomes chronic that is a serious condition that can lead to GERD It’s worth talking to a healthcare provider about your symptoms. Get treated from the best diagnostic centre near you and improve your well-being.









