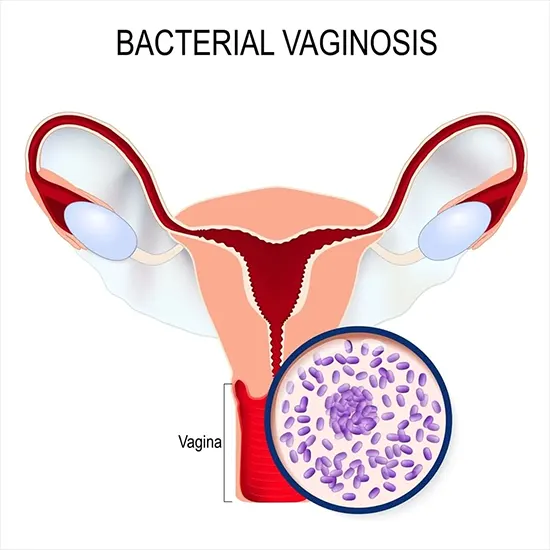
An overabundance of the normal vaginal flora is the root cause of bacterial vaginosis. Most frequently, this manifests clinically as increased, fishy-smelling vaginal discharge.
An overabundance of the normal vaginal flora is the root cause of bacterial vaginosis. Most frequently, this manifests clinically as increased, fishy-smelling vaginal discharge. Normally, the discharge itself is thin and either grey or white. Women who have been diagnosed with bacterial vaginosis are at a higher risk of contracting other STIs, and pregnant women are at an increased risk of giving birth too soon.
An excessive proliferation of the typical vaginal flora is the source of the disorder known as bacterial vaginosis. Increasing vaginal discharge with a fishy odour is the most typical clinical manifestation of this condition.Usually thin and either grey or white, the discharge itself is.Women who have been given a bacterial vaginosis diagnosis are more likely to contract other STIs, and pregnant women are more likely to give birth early.
Etiology
Despite not being a sexually transmitted disease, bacterial vaginosis, the exact function of transmissibility is still not fully known. The natural balance of the bacterial flora within the vagina may be altered by the transmission of bacteria between people during sexual activity, and this imbalance appears to be what causes bacterial vaginosis.
This illness is usually caused by a reduction in the normal Lactobacilli that produce hydrogen peroxide and an excess of anaerobic bacteria.Gardnerella vaginalis spreads between females who have sex, either directly through mucous membrane contact or indirectly through shared sex objects.
Because it was thought that the Gardnerella bacterium was to blame for this ailment, bacterial vaginosis was formerly referred to as Gardnerella vaginitis.The term "bacterial vaginosis," a more recent terminology for the ailment, helps to emphasise the possibility that a number of different bacteria that naturally exist in the vagina could proliferate excessively and result in the illness.
Epidemiology
It is believed that between 5 and 70% of women will experience bacterial vaginosis, the most prevalent vaginal infection among women of reproductive age.It's interesting to note that this illness is discovered to be least prevalent in Asia and Europe and most prevalent in some regions of Africa globally.About 30% of women in the United States between the ages of 14 and 49 are afflicted; however, rates vary significantly among different ethnic groups and are most prevalent in non-white women (51% African Americans, 32% Mexican Americans).
Epidemiological research revealed that women are more likely to report bacterial vaginosis if they have had several sexual partners, are single, first started having relations at a young age, work as commercial sex workers, or routinely engage in douching.
Pathophysiology
A change in the most prevalent kind of bacteria present as well as an increase in the overall number of bacteria present characterise the imbalance of the normally existing vaginal flora that leads to bacterial vaginosis.Species of Lactobacilli predominate in the typical vaginal microbiome.A decrease in the total quantity of Lactobacilli is linked to bacterial vaginosis. Although the exact
cause of most bacterial vaginosis infections is unknown, Gardnerella vaginalis is likely to be the first to infect the vagina, forming a biofilm that then permits the growth of other opportunistic bacteria.
Because BV makes it possible for other vaginal bacteria to potentially enter the upper genital tract, there is a link between Vaginosis (BV) Rapid and a higher risk for future STIs.In addition, BV causes an increase in endotoxin release that stimulates cytokine and prostaglandin production in the vagina as well as the presence of enzymes that impair the host leukocytes' capacity to combat infection.
Histopathology
A moist mount of vaginal fluid is examined under a microscope as the defining feature of this diagnosis. Clue cells, which are cervical epithelial cells embedded with rod-shaped bacteria, are what distinguish bacterial vaginosis from other genital infections.
Symptoms
Most bacterial vaginosis patients complain of foul-smelling vaginal discharge when they first visit. After sexual activity, this frequently becomes more obvious. Dysuria, dyspareunia, and vaginal pruritus are among additional symptoms that may exist; nevertheless, many affected women may not exhibit any symptoms at all.
Vaginal douching, many relationships, recently taking antibiotics, smoking cigarettes, and using an intrauterine device are risk factors for bacterial vaginosis.
In order to evaluate the vaginal discharge's features and to rule out other illnesses that appear similarly, such as trichomoniasis, chlamydia, herpes simplex virus, gonorrhoea, candidiasis, and cervicitis, a proper physical examination must also include a pelvic exam. Furthermore, bacterial vaginosis is a risk factor in and of itself for pelvic inflammatory disease, HIV, STIs, and other obstetric diseases.Due to this, it's crucial to check for cervical motion pain and friability as well.
Diagnosis
A vaginal swab of the cervical region or discharge is often taken to confirm the clinical suspicion of bacterial vaginosis. This sample is then turned into a wet mount slide to be examined under a microscope.The swab could have an abnormally high vaginal pH (more than 4.5), clue cells on a wet mount, and a positive sniff test.Utilising pH paper and contrasting it with colour controls can help determine the vaginal pH.
When a drop of sodium chloride solution is applied to a wet mount slide, the typical clue cells can be seen when the slide is inspected under a microscope.
The smell test is carried out by adding a little amount of potassium hydroxide to the microscope slide containing the vaginal discharge. If a distinctive fishy odour is discovered, the test is deemed positive. To confirm the diagnosis of bacterial vaginosis, often two of these positive tests are required in addition to the presence of the recognisable discharge. If there isn't any discharge, then the diagnosis can only be made if all three of these conditions are met.
Treatment management
Even though up to 30% of bacterial vaginosis cases may clear up on their own, this condition can also be managed with either clindamycin or metronidazole. Whether administered Gram Stain vaginally or taken orally, these drugs are both efficacious. Both can be used by pregnant women without any problems.The initial round of antibiotics does not improve the condition of about 10 to 15 percent of women, and they may need further care. Partners do not need to be treated for this condition because it is not a sexually transmitted infection (STI), and there is no chance of sexual transmission.
A thorough physical examination can help to narrow the differential diagnosis and aid to rule out other illnesses with similar symptoms, like the herpes simplex virus. Cervicitis can be checked for using a speculum exam, and candidiasis or trichomoniasis can be checked with a wet mount of the vaginal discharge.Chlamydia and gonorrhoea can be cultured from additional cervical samples.
According to several research, pregnant women with symptoms of bacterial vaginosis should begin taking clindamycin before 22 weeks of pregnancy in order to lower the chance of labour occurring before 37 weeks. To prevent negative effects like premature birth, the general public should either be screened for or treated for bacterial vaginosis, however there is still no clear agreement on this. Women who are asymptomatic should not currently be screened for bacterial vaginosis; however, symptomatic women should be tested and treated.
Enhancing healthcare outcomes
In clinical practise, BV frequently manifests. When dealing with BV patients, medical professionals and nurse practitioners should always check for the existence of additional STIs. Additionally, having BV while pregnant is linked to a high likelihood of premature births and spontaneous abortions.
Thus, it is crucial to conduct a BV pregnancy screening . Women with BV who receive treatment have satisfactory results, although delaying treatment increases the risk of morbidity.









