Bartonella is a Gram-negative intracellular facultative bacterium commonly implicated in zoonotic diseases worldwide. To date, approximately 20 species of Bartonella have been isolated, of which Bartonella henselae, Bartonella...
Bartonella is a Gram-negative intracellular facultative bacterium commonly implicated in zoonotic diseases worldwide. To date, approximately 20 species of Bartonella have been isolated, of which Bartonella henselae, Bartonella quintana, and Bartonella bacillus formis are commonly associated with human infections.
Trench fever, also called 5-day fever, was first reported in European soldiers. Trench fever is transmitted by body lice and is known to occur only in humans.
When a railway was constructed from Lima to Oroya, Peru, in 1870, Oroya fever was first documented. The fever outbreak killed thousands of workers and was named Oroya fever after where it was first reported. Some workers who survived the outbreak developed Peruvian warts, nodular ulcerative skin lesions.
It is commonly reported in the mountains of Peru, Colombia and Ecuador in South America. In 1885, Daniel Carrion, a Peruvian medical student, was vaccinated from Veruga and died of Oroya fever.
Causes
Cat-scratch disease, caused by Bartonella henselae, is the most commonly caused infection by Bartonella species. Bartonella bacilliformis causes Oroya fever and Peruvian warts, and Bartonella quintana is associated with trench fever. B. angiomatosis, which is the disease that causes AAS, is known to produce severe anaemia brought on by the death of red blood cells, severe enlargement of the spleen and liver, bleeding in the lymph nodes, and a high fever accompanied by blood vessel destruction. Without treatment, mortality is 40%.
Epidemiology
According to reports, there are 9.4 instances of cat scratch disease among children aged 5 to 9 and 6.4 cases per 100,000 adults globally. Incidence levels peak in January, late summer, and autumn in the southeast of the United States.
Epidemics and sporadic outbreaks of trench fever have been reported in several countries around the world since the early 20th century, with the largest global epidemics reported during World Wars I and II. It's a world war. Homeless people are more exposed to pathogens and are most at risk of contracting trench fever.
Infections with Bartonella bacilliformis are endemic in Peru, Colombia, and Ecuador, but sporadic cases have occurred in Chile, Chile, Guatemala, and Bolivia.
Pathophysiology
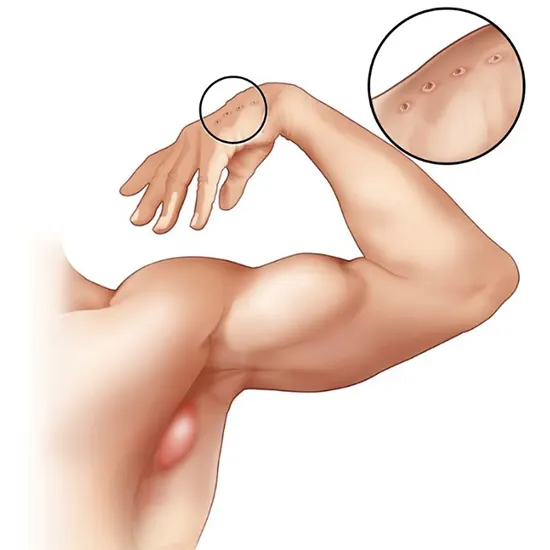
Cat-scratch disease was previously thought to be transmitted by scratches or bites of infected cats. Cats and cat fleas (Ctenocephalides felis) act as vectors for cat-scratch disease.
Recent studies have shown that other arthropod vectors such as ticks, lice, chiggers and mosquitoes are also involved in the spread of the disease among humans by Bartonella quintana, the causative agent of trench fever. . Bartonella bacillusformis is transmitted through the bite of a female Susukifly ruzomia.
Once in the body, Bartonella targets CD34+ cells, specialized white blood cells that act as precursors to endothelial cells, the cells that line blood vessels and other tissues. After entering the cell, it prevents the cell from self-destructing and creates a vacuole, a protective cyst, around itself.
An endotoxin called lipid A is commonly found in the outer membrane of Gram-negative bacteria and is the major virulence factor of Bartonella. The organism's ability to invade erythrocytes and endothelial cells plays a major role in the pathogenesis of disease processes.
Organisms alter their immune systems to make the host more susceptible to infection by other bacterial pathogens. After this acute phase, the organism invades intravascular, lymphatic, and other organ systems of the body, contributing to multiple manifestations of the disease.
Evaluation
Classic criteria for CSD diagnosis
(i) Close contact with or a scratch or bite from a cat.
(ii) Typical CSD histology (granuloma with central pyogenic abscess, not specific enough to make a CSD diagnosis),(with no lymphoid hyperplasia).
(iii) Immunofluorescence for antibodies to serology B positive by physician. Hensela.
Diagnosis of CSD must be based on a combination of epidemiological, histologic, and bacteriologic criteria, as no single criterion can be considered the gold standard.
Commonly used diagnostic methods for diagnosing Bartonella infection include serology, culture, histopathology, and polymerase chain reaction.
There are 5 blood tests
PCR DNA detection, ELISA and IFA assays, Western blot, and culture. However, it should be emphasized that Bartonella is often present only intermittently in the peripheral blood (bacteremia) of infected animals.
Direct detection method
1. Isolation in culture.
2. Detection of pathogen antigens.
3. PCR detection of nucleic acids (DNA).
4. Visualization with special coloring.
Indirect detection method
1. Serology - detection of antibodies to pathogens.
2. Detection of cellular immune responses to pathogens - Bartonella skin test. no longer used.
It is possible to culture the bacteria in order to get a certain diagnosis, but this is a time-consuming and expensive operation that can take up to 21 days to complete. Bartonella is very slow growing, fussy and difficult to primary isolate, colonies being detected on blood agar plates only after 1-4 weeks of incubation.
Bartonella spp. are difficult to cultivate, so cultivation is not routinely recommended. Using an enzyme-linked immunosorbent assay or an indirect fluorescence assay, serology is the best initial test.
Advanced diagnostic techniques such as PCR on lymph nodes and other materials are used to detect Bartonella. PCR offers the advantage of high specificity and rapid discrimination, but lacks sensitivity ranging from 43% to 76%.
The sensitivity of PCR using lymph node tissue or aspirate samples is 30-60% for CSD. Polymerase chain reaction can detect different Bartonella species. It has high specificity but less sensitivity than serology.
Treatment for disease
Treatment for cat scratch disease depends on the clinical presentation of the disease. Patients presenting with mild symptoms such as lymphadenopathy and fever usually did not receive antimicrobial therapy due to the self-limiting nature of the disease.
However, studies have shown that using a single antimicrobial regimen significantly reduces the duration of symptoms. Commonly used antibiotics are azithromycin, ciprofloxacin, gentamicin, trimethoprim-sulfamethoxazole, and rifampin.
For individuals with severe lymphadenopathy, oral azithromycin 500 mg on day 1 and 250 mg on days 2–5. For retinitis, oral doxycycline 100 mg twice daily for 4–6 weeks and oral rifampin 300 mg twice daily for 4–6 weeks.
B. quintana-associated trench fever or chronic bacteremia can be treated with oral doxycycline 200 mg once daily for 4 weeks and intravenous gentamicin 3 mg/kg for 2 weeks.
Bacterial angiomatosis and purpura hepatis with oral erythromycin 500 mg 4 times daily for 3-4 months.
Documented Bartonella culture-positive endocarditis should be treated with doxycycline 100 mg orally for 6 weeks and gentamicin 3 mg/kg/day intravenously for 14 days.
Oral rifampin 300 mg twice day and oral doxycycline 100 mg twice daily are the recommended treatments for neuroretinitis and CNS involvement. There are no controlled clinical trials comparing untreated and antibiotic-treated groups.
However, retrospective case series consistently associated antibiotics with accelerated visual recovery and improved visual outcome. Corticosteroid use in CSD with ocular involvement has had mixed results.
Ciprofloxacin is used along with chloramphenicol as a first-line drug for the treatment of Oroya fever, and ceftriaxone is a highly effective alternative. Rifampin, ciprofloxacin, and chloramphenicol are recommended alternatives to azithromycin in the treatment of verruga peruana.
Differential diagnosis
- Atypical mycobacteria.
- Coccidioidomycosis and valley fever.
- Leishmaniasis.
- Lyme disease.
- Lymphogranuloma (LGV).
- Nocardiosis.
- Sarcoidosis.
- Sporotrichosis.
- Syphilis.
- Toxoplasmosis.
Prevention from disease
- Avoid cat scratches, bites and licks, especially from kittens and feral cats. For those with compromised immune systems, this is especially crucial.
- After handling the cat, quickly wash your hands.
- Ask your veterinarian about flea prevention products for cats. (Do not use products containing permethrin on your cat).
- Keep cats indoors and away from feral cats. Do not get a cat under the age of 1 if you have a compromised immune system.









