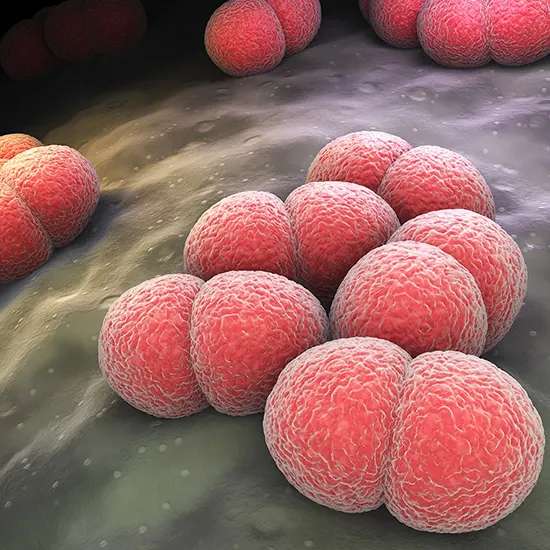
The pathogen Neisseria is responsible for the dangerous bacterial infection known as meningococcal disease. It may also result in septicemia, a potentially fatal bloodstream infection, and meningitis, an inflammation of...
Introduction to Meningococcal Disease : The pathogen Neisseria is responsible for the dangerous bacterial infection known as meningococcal disease. It may also result in septicemia, a potentially fatal bloodstream infection, and meningitis, an inflammation of the membranes that surround the brain and spinal cord.
Rapid onset and progression of meningococcal disease, which can be fatal, can have long-term health effects on survivors. It can be transmitted by kissing, sneezing, coughing, or other close contact with an infected individual.
Causes of meningococcal infection
The bacteria Neisseria , which can penetrate the lining of the brain and spinal cord as well as the bloodstream and produce meningitis or septicemia, is the cause of meningococcal illness.
Close physical contact with an infected individual, such as kissing, sneezing, coughing, or sharing personal things like water bottles or cutlery, can spread the germs. Additionally, exposure to respiratory or pharyngeal secretions from an infected person might spread it. Meningococcal infection does not necessarily result from contact with the bacteria because it depends on a number of variables, including the host's immune system and the strain's aggressiveness.
Meningococcal infection is more likely in those who live in crowded or communal environments, have weaker immune systems, travel to areas with high meningococcal illness rates, or attend major social gatherings like music festivals or college dorms. Meningococcal infection must be treated with antibiotics as soon as possible in order to avoid spreading.
Symptoms of meningococcal infection
various age groups may experience various meningococcal disease manifestations. Children as young as infants and toddlers may exhibit symptoms like irritability, poor eating, and a high-pitched cry. Headache, nausea, and a stiff neck are some of the symptoms. In extreme circumstances, the infection may spread quickly, resulting in sepsis and septic shock.
A crucial sign to watch out for is the skin rash linked to meningococcal disease since it frequently serves as an indicator of the infection. The rash might not disappear when pushed with a glass or another object (referred to as "non-blanching") and can arise anywhere on the body. A non-blanching rash is an indication of a medical emergency, therefore anyone who gets it should see a doctor right away.
It is important to remember that not everyone who acquires meningococcal disease will have all of the following symptoms:
Others may experience severe symptoms that appear suddenly, while some people may experience moderate symptoms that are mistaken for the flu or another common virus.
Meningococcal disease symptoms must be understood, especially if a person has risk factors for the illness, such as recent travel to high-risk locations or close contact with an infected person.
Diagnosis of Meningococcal infection
Physical exam: During the physical exam, a doctor or healthcare professional will look for signs of meningitis or septicemia, such as a fever, headache, stiff neck, and skin rash. Inquiries concerning the patient's medical background, recent travel, and any contact with meningococcal illness will also be made.
Medical history: A thorough medical history is gathered in order to assess the patient's symptoms, length of sickness, and risk factors for meningococcal disease, such as recent travel, contact with sick people, or vaccination records.
Laboratory tests: Several laboratory tests, such as the following, are used to identify meningococcal infection:
Blood tests: These exams are capable of detecting the Neisseria germs in the bloodstream and calculating the body's level of inflammation.
Cerebrospinal fluid (CSF) is taken from the spine during a lumbar puncture for study. White blood cells, germs, and other signs of meningitis can all be found via CSF analysis.
Imaging studies: x-ray, CT scans or MRIs may occasionally be recommended in order to determine the extent of edema and damage to the brain and spinal cord.
Based on the results of these diagnostic tests, the doctor can make a firm diagnosis of meningococcal infection and determine the best course of treatment. Prompt diagnosis and treatment are necessary to increase the likelihood of a full recovery and reduce the risk of complications.
Types of Meningococcal Infection
Meningococcal infections typically come in two different forms:
Meningococcal meningitis : Inflammation of the meninges, the protective membranes that encircle the brain and spinal cord, characterises this kind of meningococcal infection. The symptoms of meningococcal meningitis include fever, headache, stiff neck, nausea, vomiting, disorientation, and light sensitivity.
Meningococcal septicemia : Meningococcal bloodstream infection is another name for this kind of meningococcal illness. When bacteria get into the bloodstream and start to infect people severely, it happens. Fever, chills, quick breathing, rapid heartbeat, low blood pressure, and a rash that doesn't go away when touched are all signs of meningococcal septicemia. Organ failure, shock, and even death are possible in extreme circumstances.
Neisseria is the bacterium that causes both forms of meningococcal infections. The bacterium can be shared by close contact with an infected individual, such as kissing or sharing utensils or drinks, EEG as well as through respiratory and throat secretions like coughing and sneezing. Antibiotics can be used to treat meningococcal infection, but early detection and intervention are crucial to improve results and lower the risk of sequelae. There are also various meningococcal infection vaccines available.
Treatment and management of meningococcal infection
Antibiotics and supportive care are often used in combination to treat and manage meningococcal infections. For better results and a lower chance of problems, prompt treatment is Blood Culture crucial. The course of action will depend on the degree of the infection, the patient's age and general condition, as well as the infection itself.
Antibiotics : Antibiotics are used to kill the microorganisms causing the infection, such as penicillin, ceftriaxone, and ciprofloxacin. The type of antibiotic will depend on the patient's medical history, allergies, and how susceptible the bacteria are to the medication.
Supportive treatment : To control symptoms and avoid complications, supportive care techniques such IV fluids, oxygen therapy, and pain management may be required. In order to support organ function, patients with severe infections may need critical care and artificial breathing.
Meningococcal infection patients should be isolated in order to stop the bacterium from spreading to others. The patient may be kept in a private room, required to wear personal protective equipment, and have a limited number of visitors as isolation precautions.
Vaccination : Serogroups A, B, C, W, and Y meningococcal infections can all be prevented with certain vaccines. For some groups, such as kids, teenagers, college students, service members, and anyone travelling to high-risk locations, vaccination is advised.
Contact tracing : To stop the spread of the germs, it may be necessary to assess and treat close contacts of meningococcal infection patients with antibiotics.
Follow-up : After a meningococcal infection has been treated, patients should be checked for any long-term side effects like hearing loss, cognitive decline, or limb amputation.
Public Health consideration and outbreak management
Case management : Healthcare professionals must notify public health authorities of any suspected or confirmed cases of meningococcal infection. To avoid problems and lower the risk of transmission to others, patients with meningococcal infections should receive rapid diagnosis and treatment.
Isolating infected persons and using proper care, such as antibiotics, can help stop the spread of the illness and lower the risk of life-threatening consequences. Supportive care, such as intravenous fluids, may also be used as part of the treatment to manage symptoms and prevent dehydration.
Chemoprophylaxis : Giving preventative antibiotics to people who have come into touch with an infected person can help stop the spread of the illness.
Immunisation: Immunisation is a crucial method for preventing meningococcal infection, especially in those who are at higher risk of infection, such as adolescents and young adults, as well as those with specific medical conditions.
The dissemination of correct information and the implementation of relevant public health initiatives depend on effective communication with the general public, healthcare practitioners, and other stakeholders. Information on meningococcal infection symptoms and indications is one aspect of this.
Environmental control measures: Implementing sanitation and disinfection programmes can help lower the risk of transmission by limiting the disease's ability to spread in the environment.
Meningococcal infection is a dangerous condition that can have disastrous effects. Meningococcal infection outbreaks can be managed and the disease's transmission can be stopped with the use of efficient public health measures and outbreak management techniques. Public health personnel have access to a wide variety of efficient tactics, from monitoring and case investigation to immunisation and communication.
We can safeguard our neighbourhoods and stop the spread of meningococcal infection by banding together and putting these solutions into practice, thereby enhancing everyone's health and