Vaginal cancer comes in a variety of forms, such as squamous cell carcinoma, adenocarcinoma, and melanoma. The thin, flat cells that line the surface of the vagina give rise to the most prevalent kind of vaginal cancer,...
We are stronger than vaginal cancer, let's show it who's boss - All you need to know about Vaginal Cancer-
An Overview
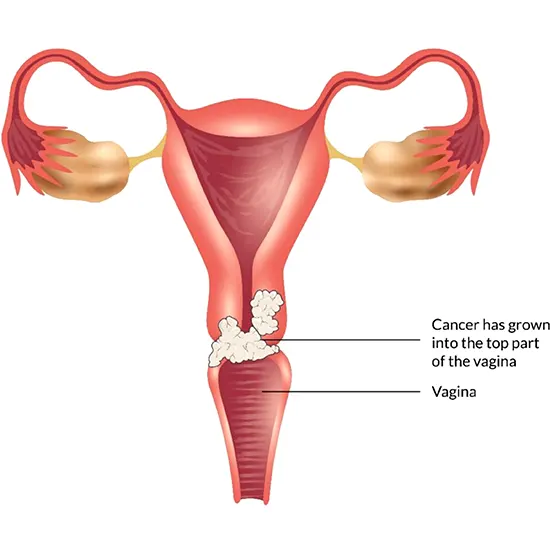
The muscle-filled tube that links the uterus to the outside of the body is called the vagina, and vaginal cancer is a rare kind of cancer that begins in the cells of the vagina.
Vaginal cancer comes in a variety of forms, such as squamous cell carcinoma, adenocarcinoma, and melanoma. The thin, flat cells that line the surface of the vagina give rise to the most prevalent kind of vaginal cancer, squamous cell carcinoma. Melanoma develops in skin pigment-producing cells, whereas adenocarcinoma does so in the glandular cells that line the vagina.
Although there is no known cause for vaginal cancer, there are several risk factors that might raise the likelihood of getting the illness. Cancer usually develops slowly over several years and is more common in women who are over the age of 60.
Chemotherapy, radiation therapy, surgery, or a combination of these treatments can all be used to deal with vaginal cancer. The stage of the disease at the time of diagnosis and the person's general health both affect the vaginal cancer prognosis.
This article will provide you with in-depth knowledge of the causes symptoms and various treatment options of Vaginal cancer.
Know the Commonness
Less than 2% of all gynecologic malignancies in the US are vaginal cancers, making them an uncommon kind of cancer.
It is predicted by the American Cancer Society that in 2022 there will be around 6,310 new instances of vaginal cancer in the US, along with approximately 1,170 related fatalities.
The chance of contracting the disease rises with age, with women over 60 having the greatest prevalence of vaginal cancer.
Vaginal cancer is also more common in women who have had a history of abnormal cervical cells or cervical cancer, exposure to the drug DES (diethylstilbestrol) in utero, a weakened immune system, smoking, and HPV (human papillomavirus) infection.
While vaginal cancer is rare, it is still important for women to be aware of the signs and symptoms of the disease, and to talk to their healthcare providers about any concerns they may have.
Understanding the risk factors can help reduce the incidence of vaginal cancer
The exact cause of vaginal cancer is not fully understood, but several known risk factors may increase the chances of developing the disease. These risk factors include:
Infection with the human papillomavirus (HPV): The HPV virus is a frequent sexually transmitted infection that can alter the cervix, vagina, and other reproductive tract cells. Vaginal cancer can be caused by certain HPV strains.
Diethylstilbestrol (DES) exposure: Throughout the 1940s and 1960s, pregnant women were given DES, a synthetic hormone, to prevent miscarriages. Vaginal cancer is more likely to occur in women who were exposed to DES when they were still growing.
Age: Females over the age of 60 are more likely to get vaginal cancer, and the likelihood of doing so rises with age.
History of Abnormal Cervical Cells or Cervical Cancer: Women who have had abnormal cervical cells or cervical cancer in the past have an increased risk of developing vaginal cancer.
Weakened Immune System: Women who have a weakened immune system, such as those who have had an organ transplant or are living with HIV, may have an increased risk of developing vaginal cancer.
Smoking: Many cancers, including vaginal cancer, have been associated with a higher risk when a person smokes.
Family history: Vaginal or cervical cancer may be more likely to strike women who have a history of the disease in their families.
Radiation Therapy: Females who went through radiation therapy to the pelvic area as part of their treatment for another cancer, such as cervical cancer, may have an increased risk of developing vaginal cancer.
Exposure to Chemicals: Women who have been exposed to certain chemicals, such as those used in the rubber industry or dry cleaning, may have an increased risk of developing vaginal cancer.
Bad Diet: An unhealthy diet with a high intake of processed foods and a low intake of fruits and vegetables may raise the chance of getting cancer, particularly vaginal cancer.
Obesity: Many forms of cancer, including vaginal cancer, are more likely to develop in people who are overweight or obese.
Chronic Vulvar or Vaginal Infections: Women who have chronic infections of the vulva or vagina may have an increased risk of developing vaginal cancer.
It's important to keep in mind that some of these risk variables, including age and family history, are immutable. Women can alter their lifestyles, such as giving up smoking, eating a balanced diet, and engaging in safe sex, to lower their chance of getting vaginal cancer. Frequent examinations and screenings with a healthcare professional may also aid in the early detection of any irregularities, which can increase the likelihood that a successful course of treatment.
Body Signals to Vaginal Cancer
Vaginal cancer symptoms and indicators can differ from person to person, and some women may even have no symptoms at all. However, some common symptoms and signs of vaginal cancer include:
Irregular vaginal bleeding: The most typical sign of vaginal cancer is this. In between cycles, after intercourse, or after menopause, it might happen.
Vaginal discharge: A woman with vaginal cancer may experience a watery, bloody, or foul-smelling vaginal discharge that is not associated with her menstrual cycle.
Pain during sex: Some women with vaginal cancer may experience pain or discomfort during sexual intercourse.
Pain in the pelvic area: Women with vaginal cancer may experience pain or discomfort in the pelvic area, including the lower back, buttocks, or legs.
Lump or mass in the vagina: A woman with vaginal cancer may feel a lump or mass in the vaginal wall.
Itching or burning in the vagina: Women with vaginal cancer may experience itching or burning in the vagina, which can be a sign of an illness.
Pain or discomfort in the vaginal area: Women with vaginal cancer may experience pain or discomfort in the vaginal area, which can be a sign of a tumor pressing against nearby nerves or organs.
Difficulty urinating: Women with vaginal cancer may experience difficulty urinating, which can be a sign of a tumor pressing against the bladder or urethra.
Unexplained weight loss: Unexplained Weight loss: Weight loss that is unexplained in women with vaginal cancer may indicate that the disease has progressed to other bodily organs.
It's important to note that these symptoms and signs may also be present in other conditions such as infections, cysts, or benign tumors.
Early detection saves lives, get screened for vaginal cancer today
There are several diagnostic tests that healthcare professionals may use to diagnose vaginal cancer. To receive a correct diagnosis and treatment plan, it is crucial to consult a doctor.
Let's examine each in more detail:
Pelvic Exam: An examination of the vagina, cervix, uterus, ovaries, and fallopian tubes is known as a pelvic exam. A medical practitioner will search for any anomalies, such as lumps or masses, that might be signs of vaginal cancer during this examination.
Pap Test: A Pap test is a screening procedure that looks for abnormal cervix cells. The presence of abnormal cells in the vagina may be a sign of malignant or precancerous tissue.
Biopsy: A biopsy is a process in which a little sample of tissue from the vagina is taken and submitted to a lab for examination. A biopsy can identify the kind and stage of cancer as well as confirm the existence of malignant cells.
Colposcopy: During a colposcopy, a medical expert uses a specialized device to look for abnormal cells in the vagina and cervix. If aberrant cells are discovered during the process, a biopsy may be performed.
MRI: An MRI (Magnetic Resonance Imaging) is a radiography procedure that produces precise pictures of the vagina and tissues around using a high magnetic field and radio waves. This examination can aid in determining a tumor's size and extent.
CT Scan: A CT (Computed Tomography) scan is a radiographic procedure that produces in-depth pictures of the body using X-rays and computer technologies.
PET Scan: A PET scan, also known as positron emission tomography, is a radiographic test that produces pictures of the body using a specific dye and a scanner. This examination can reveal whether cancer has spread to other bodily regions.
Blood Tests: Blood testing can assist in identifying certain signs that could point to the existence of malignancy. These tests can be useful to track therapy and spot recurrence but are not used to diagnose vaginal cancer.
Test for Human Papillomavirus (HPV): Vaginal cancer risk might rise in the presence of the sexually transmitted disease human papillomavirus (HPV).
Vulvoscopy: A colposcopy is a procedure in which a healthcare professional uses a special instrument to examine the vulva (the external genitalia) for any abnormalities, such as warts or lesions that may indicate the presence of vaginal cancer.
CA-125 Test: CA-125 is a protein that may be elevated in women with advanced vaginal cancer. This test is not used to diagnose vaginal cancer but may be used to monitor treatment and detect recurrence.
It's crucial to remember that not every woman with a suspicion of vaginal cancer will require all of these tests. The particular tests used will depend on the patient's symptoms, medical background, and outcomes of the physical examination. A doctor will collaborate with the patient to create a personalized diagnostic strategy that takes into account all of their unique requirements.
Discovering different approaches to Treat Vaginal Cancer
Vaginal cancer can be treated using a combination of medicines, surgery, and radiotherapy. The course of treatment is determined by cancer's stage, the tumor's location, and the patient's general health.
Medicines:
Chemotherapy
Chemotherapy is a sort of drug used to treat vaginal cancer. Drugs that either destroy cancer cells or stop their proliferation are used in this procedure. To increase its efficiency, chemotherapy is frequently administered in conjunction with radiation treatment.
Hormone therapy
It may also be used in some cases of vaginal cancer that are hormone-sensitive. Although estrogen and progesterone can promote the development of some cancer cells, this form of treatment works by preventing their effects. Hormone therapy drugs that may be used for vaginal cancer include tamoxifen and aromatase inhibitors
Surgery: Surgery is an option for early-stage vaginal cancer. The purpose of surgery is to eliminate the tumor and any surrounding healthy tissue. A simple hysterectomy may be enough for tumors that are confined to the vagina, while more extensive surgery may be necessary for tumors that have spread to nearby organs or lymph nodes.
Here are some examples of surgeries that may be used to treat vaginal cancer:
Local excision: A local excision is a surgical procedure that involves the removal of the cancerous tissue and a margin of healthy tissue around it. This type of surgery may be used for early-stage vaginal cancer that has not spread beyond the vagina.
Pelvic exenteration: A pelvic exenteration is a complex surgical procedure that involves the removal of the uterus, cervix, vagina, ovaries, and nearby lymph nodes. This type of surgery may be used for advanced-stage vaginal cancer that has spread to nearby organs, such as the bladder or rectum.
Lymphadenectomy: A lymphadenectomy is a surgical operation in which the lymph nodes in the pelvic region are removed. This type of surgery may be done as part of a radical hysterectomy or pelvic exenteration to remove cancerous lymph nodes and prevent the spread of cancer to other parts of the body.
Vaginectomy: A vaginectomy is a surgical procedure that involves the deduction of all or portion of the vagina. This type of surgery may be used for advanced-stage vaginal cancer that has spread beyond the vagina and cannot be treated with radiation therapy.
Radiotherapy: Radiation therapy uses high-energy beams of radiation to kill cancer cells. It is the most common treatment for vaginal cancer, particularly for larger tumors or those that have spread beyond the vagina.
Targeted therapy: Targeted therapy is a type of cancer treatment that uses drugs to target specific molecules or pathways that are involved in the development and spread of cancer cells.
Palliative care: The objective of palliative care is to improve the grade of life for patients with life-threatening diseases, such as cancer. It tries to treat physical symptoms including pain, nausea, and weariness as well as give patients and their families psychological and spiritual support. If a patient is not a candidate for curative therapy, palliative care can be utilized alone or in conjunction with other vaginal cancer therapies.
Clinical trials: Clinical trials are research projects that look at potential vaginal cancer therapies. These could entail experimenting with brand-new medications, radiation therapy methods, or surgical techniques. Clinical trials are a crucial component of improving cancer care and may provide patients access to cutting-edge, perhaps life-saving therapies.
Vaginal cancer doesn't discriminate, but neither do we in the fight against it.









