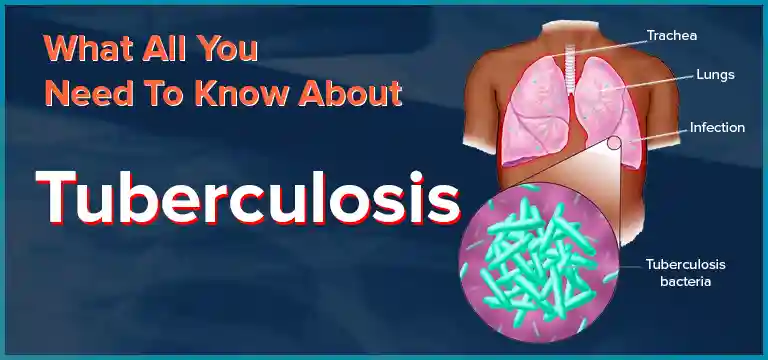
Tuberculosis or TB is considered to be an infectious disease that is in general caused by the organism- Mycobacterium tuberculosis (MTB) bacteria. Normally it is seen that Tuberculosis affects the lungs, however, other...
Tuberculosis (TB) Overview:
Tuberculosis or TB is considered to be an infectious disease that is in general caused by the organism- Mycobacterium tuberculosis (MTB) bacteria.
Normally it is seen that Tuberculosis affects the lungs, however, other parts of the body can be affected
Latent Infections: When most infections do not show any symptoms, in this case it is known as latent tuberculosis
It is seen that around 10% of the latent infections progress to an active disease state which, if are left untreated, would end up killing about half of the patients affected.
Active Infection: Active tuberculosis is known to be a multiorgan disease that is caused by a primary infection or even a reactivation of latent tuberculosis, as mentioned above.
Symptoms of TB
Typical symptoms of active TB include the following:
- Chronic cough with blood-containing mucus
- Fever
- Night sweats
- Weight loss
It was historically known to be called as consumption due to all the weight loss which is associated with the disease Infection of the other organs that can get affected. We would be discussing the effect of TB and the wide range of symptoms in multiple organs and systems
Mode of Spread: The Tuberculosis is generally spread from one person to another through air when patients have active TB in their lungs cough, when they spit, or speak, or sneeze.
Note: Patients with latent TB will not spread the disease.
Active infection is seen to usually occurs more often in patients suffering from with HIV/AIDS and in individuals who smoke
Other Etiologic Agent or the Causative Organism
MTBC bacteria include slowly growing, and host-associated bacteria such as:
- Mycobacterium tuberculosis- Most common
- Mycobacterium bovis
- Mycobacterium microti
- Mycobacterium africanum
- Mycobacterium pinnipedii
- Mycobacterium caprae
- Mycobacterium canettii
These organisms are responsible in causing tuberculosis in both humans and animals.
Epidemiology of TB
It is important to understand that in 2016- there were 6.3 million new cases of TB Out of which 95% were from the developing countries
In this Asian population itself being – 6.5 million in number.
Innate Resistance to Infection
The Mycobacterium tuberculosis (Mtb) infection is seen to be can be cleared by the innate immune (Body’s first line of defense against pathogens) system before the initiation of an adaptive immune response (second time exposure or memory response and response post vaccination)
The innate protection thus requires a number of robust cell and autonomous responses from different host immune cell types.
Major innate immune cell types that involved in tuberculosis (TB) infection are as follows:
- Macrophages
- Dendritic cells (DCs
- Neutrophils
- Natural killer (NK) cells
Clinical Manifestation of Tuberculosis
The Primary (initial) infection is considered to be usually indicated by the tuberculin skin test (TST) or the interferon-gamma release assay (IGRA) conversion.
This is seen reflecting a delayed type of hypersensitivity reaction to various protein products produced by M. tuberculosis.
The TST conversion then usually occurs post 3–6 weeks after the 1st exposure/infection
Primary infection
The primary infection of TB usually remains undiagnosed in majority of cases, usually it is seen that the symptoms are as follows:
- Mild
- Non-specific
- Usually self-resolving
Histopathology Picture: A primary or (Ghon) complex is formed, which consists of granuloma, characteristically in the middle or in the lower zones of the lung (primary or Ghon focus) in combination with the transient hilar and/or paratracheal lymphadenopathy (swelling of lymph nodes) with some overlying pleural reaction.
The primary complex is seen resolving within a few weeks or even months,
X-ray Detection: Signs of fibrosis and calcification detectable on the chest X-ray, even after the primary complex is resolved.
In general, risk of the disease progression following a primary infection is quite low, but the young children and the immunocompromised patients are considered to be at increased risk.
Pulmonary TB
The TB symptoms are typically gradual in onset and the duration is seen to vary from weeks to even months, although more acute onset could occur in very young children or even in immunocompromised individuals.
The typical triad includes the following 3 symptoms:
- Fever
- Night sweats
- Weight loss
Parenchymal
- The Cough in this case might be non-productive (without mucus) or patient might have the sputum that could be either mucoid or mucopurulent, or blood-stained and have also massive haemoptysis (with blood present).
- Other symptoms might include the following: chest pain, in patients with the sub pleural involvement, or dyspnoea (difficulty in breathing) however, it is rare.
Endobrochial
- Endobrochial TB is known to be a specific form of pulmonary TB the affects the trachea and also the major bronchi.
- It can be often misdiagnosed as either bronchial asthma or even as bronchial malignancy.
Intra- thoracic Lymph node disease
- Following the first-time infection, the regional lymph nodes are said to form part of the primary (Ghon) complex.
- Then, progressive disease might occur within the affected regional lymph nodes and is usually seen in the young children.
- The Symptoms are quite similar to other forms of pulmonary TB, although here the cough is seen to be rarely productive (non-mucus containing) or the sputum blood-stained.
Extra pulmonary
- The Pleural fluid here is mostly seen as lymphocytic (high number of WBC) with high protein content.
- The Bacillary load (bacterial load/ amount) is considered to be generally low and the smear is typically negative, though this might be higher in the HIV positive patients, in whom the diagnostic yield from the smear might be as high as 50 %
Miliary TB
- The Miliary TB can occur during the primary infection and in mostly in the post-primary disease.
- It indicates the dissemination of the disease and this arises from hematogenous spread of the bacilli, which might then occur shortly after the primary infection or from any other active disease site.
- Note: In Children- Mostly Primary Infection Is observed.
- In Adults- Mostly Hematogenous Spread is observed.
TB of Upper Airways
- This form of the disease may involve the following: larynx, pharynx and epiglottis
- Nearly, it is always seen as a complication of advanced cavitatory TB.
Genitourinary TB
The following symptoms of the following are observed:
- Urinary frequency
- Dysuria (painful urination)
- Nocturia( frequent urine urge at night)
- Hematuria and abdominal pain
Skeletal TB
- Spinal TB: Potts Disease or tuberculosis Spondylitis
- Here, the Upper thoracic spine is the most common site of spinal TB in children.
- While, the Lower thoracic and upper lumbar vertebrae are seen to be affected in adults.
- TB of the knee: Pain in the joint pain and inflammation
- TB of hip joints: Involving head of the femur bone
Tuberculosis Meningitis and Tuberculoma
- An uncommon manifestation of TB of CNS, presents as one or more- space occupying lesions and causes - Seizures and focal signs.
Gastrointestinal TB
- Abdominal pain, appendicitis, fever, weight loss, anorexia, and stimulation of Crohn’s disease are presenting symptoms.
Pericardial TB
- Develops frequently in HIV- infected patients
- Mortality rate as high as 40%
- May eventually cause cardiovascular problems’
Complications of TB
Tuberculosis infection can also cause many complications like:
- Joint damage
- Lung damage
- Infection or damage of the bones, spinal cord, brain, or lymph nodes.
- Liver or kidney problems
- Inflammation of the tissues around the heart
What kinds of tests are used to diagnose tuberculosis?
There are generally kinds of the screening tests for TB:
- Monteux tuberculin skin test (TST)
- Blood test, called the interferon gamma release assay (IGRA).
- Acid Fast Bacilli (AFB)
During the test:
For TST, a healthcare provider would inject a small amount of the substance called the purified protein derivative (PPD) under the skin of the forearm.
For the next test called IGRA, the healthcare provider would draw some amount of blood and would then send this sample to the respective lab.
After the test:
After around two to three days, one should go back to the healthcare professional, to evaluate the injection site.
Other Tests
Moreover, there are more tests that are used to determine if an infection is active or if the lungs are infected which include the following:
- Lab tests on sputum and lung fluid.
- Chest X-ray.
- Computed tomography (CT) scans.
How Is Tuberculosis Treated?
The TB infection and the disease are treated with the following drugs:
- Isoniazid (Hyzyd®).
- Revampingz (Rifadin®).
- Ethambutol (Myambutol®).
- Pyrazinamide (Zinamide®).
- Rifapentine (Priftin®).
You should take all the medication that the provider would prescribes, or not all of the bacteria would be destroyed
You should consume these medications for as long as advised from 9 to 12 months.
1st line of treatment: Of these approved drugs, the ones mentioned above, such as: isoniazid (INH), rifampin (RIF), ethambutol (EMB), and pyrazinamide (PZA) are considered to be the first-line anti-TB drugs and thus, they form the core of this standard treatment regimens
While, Rifabutin (RBT) and rifapentine (RPT) might be considered first- line drugs under some certain circumstances.
Directly Observed Therapy (DOT)
The DOT is preferred core management strategy which is recommended by CDC for the treatment of the TB disease and sometimes also for latent tuberculosis infection (LTBI) treatment.
Nearly, all treatment regimens that are drug-susceptible TB disease would be given intermittently if they are directly observed.
Also, the Drug-resistant TB disease must be a daily regimen and under direct observation.
There are also no intermittent regimens for the treatment of the multidrug-resistant (MDR) TB.
Fixed-Dose Combination Drugs
The use of this fixed-dose combination capsules or the tablets facilitates this DOT administration by minimizing chance for any error through the even use of fewer tablets and this might reduce the risk of any acquired/ Multidrug resistance (MDR) since one of the medication that cannot be selectively taken.
Self-Administered Therapy
Patients on their self-administered therapy should be monitored routinely for Patient Adherence and further follow-up visits.
Why should Ganesh diagnostic and Imaging Centre be your preference for getting Tuberculosis Test done ?
At Ganesh Diagnostic and Imaging Centre, we are known for providing excellent service and care to its patients for decades. Lakhs of satisfied patients over the years!
It is an established and renowned diagnostic centre since 2001.
Their excellence is backed by NABH and NABL Accreditations.
NABH accreditation is proof of highest standard of care and service provided to the patients. NABL accreditation reflects the competency of laboratories and equipment based on some national and international standards.
Test report is available digitally too.
Ganesh Diagnostic and Imaging Centre is a one-stop solution for getting all kinds of tests done, as all services are available under one roof.
The aim of GDIC is to provide world’s finest technology at the lowest price.
The rates of scans are reasonably priced. Ganesh Diagnostic and Imaging Centre also offer FLAT 50% OFF on many tests.
Patients can rely upon test reports as reports are 100% accurate.
The cost of the Tuberculosis Tests in Delhi, at Ganesh Diagnostic and Imaging Center are as follows.
References
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4832344/
- https://en.wikipedia.org/wiki/Tuberculosis
- https://www.ncbi.nlm.nih.gov/books/NBK344404/
- http://www.cdc.gov/tb/publications/factsheets/testing/skintesting.htm.
- https://www.cdc.gov/tb/education/corecurr/pdf/chapter6.pdf
- Harrison's® Principles of Internal Medicine, 20th edition, Volume 1
AFB-Identification & Speciation MTB and MOTT by Hains Test Rs 2400 Rs 1200 BOOK NOW
C/S for Mycobacterium TB Test Rs 1000 Rs 500 BOOK NOW
GeneXpert MTB with Rifampicin Sensitivity, Qualitative PCR Test Rs 3000 Rs 1500 BOOK NOW
GeneXpert MTB with Rifampicin Sensitivity, Quantitative PCR Test Rs 2860 Rs 1430 BOOK NOW
Genexpert Ultra (Next Generation) MTB PCR Test Rs 2200 Rs 1650 BOOK NOW
Mycobacterium Tuberculosis Culture Test Rs 1000 Rs 500 BOOK NOW
Mycobacterium Tuberculosis MTB Rs 2000 Rs 1500 BOOK NOW
PCR TB For Semen Rs 1900 Rs 950 BOOK NOW
QuantiFERON - TB Gold Test Rs 2800 Rs 1400 BOOK NOW









