The risk increases with age, with breast cancer being most frequently diagnosed in women between the ages of 55 and 64. A patient has a better chance of being cured and the side effects of their therapy are lessened with early...
The risk increases with age, with breast cancer being most frequently diagnosed in women between the ages of 55 and 64. A patient has a better chance of being cured and the side effects of their therapy are lessened with early identification.
Though breast cancer treatments are getting better and have helped lower mortality, mammograms have a bigger overall impact on mortality reductions than early detection through treatment.
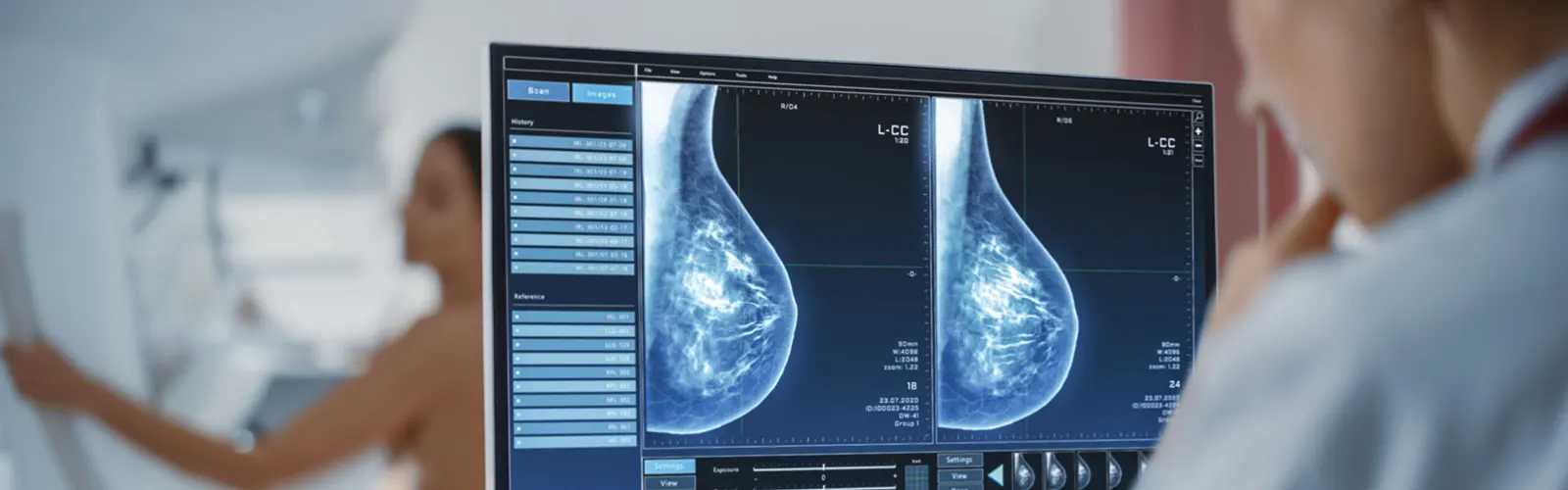
Starting at age 40, all women with an average risk for breast cancer should undergo screening, according to the American College of Radiology. Numerous techniques, including mammography, breast ultrasound, and magnetic resonance imaging (MRI), can be used to suggest the presence of breast cancer.
Types of mammography
There are mainly two types of mammography
- Screening mammogram
- Diagnostic mammogram
Screening mammogram
Mammography screening is the process of checking asymptomatic women for clinically occult breast cancer. Two views of the breast are examined during the screening test; these views are commonly referred to as the "standard views."
Although debates over the precise statistical advantages of screening mammography persist, a recent review of the literature by the Institute of Medicine recommended mammography as the most reliable screening method for finding breast cancer.
In addition, a recent analysis on screening in seven Swedish counties—roughly 33% of Sweden's population—found that women who underwent screening experienced a 40%–45% decrease in breast cancer mortality.The findings of this study showed that screening is mostly to blame for the majority of the recent decline in breast cancer mortality.
Diagnostic mammogram
When there are clinical signs, such as a palpable lump or an abnormal screening mammogram, that call for further investigation, diagnostic mammography, also known as "consultative" or "problem-solving" mammography, is carried out.
Additional breast views, such as spot compression and magnification, a correlative clinical examination, and ultrasonography, may be included in diagnostic mammography. A radiologist should always be present while a diagnostic mammography study is being conducted, with a few exceptions.
When a biopsy for a palpable lump in a woman older than 30 years old is being considered, diagnostic mammography should also be done. Prior to performing a biopsy on a palpable mass, diagnostic mammography is used to identify the clinical abnormalities and look for any additional (unexpected) lesions, such as intraductal extensions of invasive carcinomas or multifocal carcinomas.
Before performing a diagnostic mammogram, a radiopaque marker ("BB") should be placed over any areas of clinical concern in order to correlate the clinical with the imaging findings.









