A bone density test, also known as dual-energy X-ray absorptiometry (DXA) or bone densitometry, is a medical procedure used to measure the strength and density of your bones.
Introduction
A bone density test, also known as dual-energy X-ray absorptiometry (DXA) or bone densitometry, is a medical procedure used to measure the strength and density of your bones. It is primarily performed to diagnose osteoporosis, a condition characterized by low bone mass and an increased risk of fractures.
Scanning:
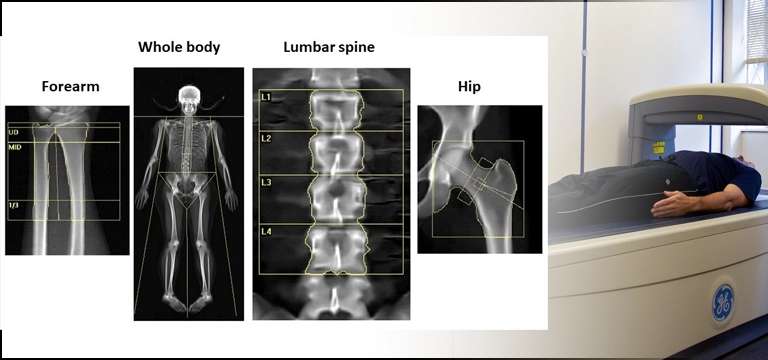
During a bone density test, a specialized X-ray machine scans specific areas of your body, usually the hip and spine, to measure the amount of mineral content, such as calcium, in your bones. The test is painless and non-invasive, involving a low dose of radiation.
Results:
The results of a bone density test are usually presented as a T-score and a Z-score. The T-score compares your bone density to that of a healthy young adult of the same sex, while the Z-score compares your bone density to that of an average person of your age and sex. A T-score of -1 or above is considered normal, between -1 and -2.5 indicates osteopenia (low bone density), and -2.5 or lower suggests osteoporosis.
Based on the results, your doctor can assess your risk of fractures and determine if you need treatment or lifestyle changes to improve your bone health. Bone density tests are typically recommended for postmenopausal women, men over 70, individuals with specific risk factors, and those already diagnosed with osteoporosis or on medications that may affect bone health.
When Should I Consider Taking a Bone Density Measurement Test?
It is generally recommended to consider taking a bone density measurement test in the following situations:
- Postmenopausal Women: Women who have gone through menopause, especially those aged 65 and older, are at a higher risk of developing osteoporosis. It is advisable for postmenopausal women to undergo a bone density test to assess their bone health.
- Men over 70: While osteoporosis is more commonly associated with women, men are also at risk, especially as they age. Men aged 70 and older can benefit from bone density testing to evaluate their bone health.
- Individuals with Risk Factors: If you have specific risk factors that increase your likelihood of developing osteoporosis, it is recommended to consider a bone density test. Risk factors include a family history of osteoporosis, a personal history of fractures as an adult, low body weight, smoking, excessive alcohol consumption, long-term use of corticosteroid medications, and certain medical conditions (such as rheumatoid arthritis or celiac disease).
- Monitoring Osteoporosis Treatment: If you have been diagnosed with osteoporosis or are undergoing treatment for the condition, regular bone density tests can help monitor the effectiveness of the treatment and track changes in bone density over time.
- Assessing Fracture Risk: In some cases, if you have experienced a fracture from a minor fall or have had a significant height loss, a bone density test can be useful in assessing your fracture risk and determining the underlying cause.
Ultimately, it is best to consult with your healthcare provider or primary care physician who can assess your individual risk factors, medical history, and recommend the appropriate timing for a bone density measurement test.
In What Conditions is Bone Density imaging done?
Bone density imaging, specifically dual-energy X-ray absorptiometry (DXA), is primarily done in the following conditions:
- Osteoporosis: DXA scans are commonly used to diagnose osteoporosis, a condition characterized by low bone density and increased risk of fractures. It helps determine the severity of the disease and assess the risk of future fractures.
- Monitoring Osteoporosis Treatment: Once diagnosed with osteoporosis, regular DXA scans may be performed to monitor the effectiveness of treatment and track changes in bone density over time. This helps healthcare providers evaluate the response to medications and lifestyle modifications.
- Osteopenia: DXA scans are also used to diagnose osteopenia, a condition characterized by lower than normal bone density but not as severe as osteoporosis. It helps identify individuals with early signs of bone loss and assess their risk of developing osteoporosis.
- Assessing Fracture Risk: DXA scans can be utilized to assess an individual's risk of fracture due to low bone density. By evaluating bone mineral density in key areas such as the hip and spine, healthcare providers can estimate the likelihood of fractures and determine appropriate preventive measures.
- Monitoring Bone Health in Medical Conditions: Certain medical conditions and treatments can affect bone health. DXA scans may be performed to monitor bone density in individuals with conditions such as hyperparathyroidism, chronic kidney disease, rheumatoid arthritis, or individuals on long-term medications that can impact bone health.
- Evaluation of Bone Health in Cancer Patients: Some cancers, as well as cancer treatments such as chemotherapy or hormonal therapies, can affect bone health. DXA scans may be used to assess bone density and guide management strategies in cancer patients.
How is the Bone density Test Done?
A bone density test, specifically dual-energy X-ray absorptiometry (DXA), is a safe and non-invasive procedure. The test procedure is described below:
- Preparation: Generally, no specific preparation is required for a bone density test. However, you may be asked to avoid taking calcium supplements or medications that contain calcium on the day of the test, as they can interfere with the accuracy of the results.
- Clothing and Positioning: You will be asked to change into a gown or wear loose, comfortable clothing without any metal objects, such as zippers or buttons, as they can interfere with the X-ray images. You will lie on a padded table, usually on your back, and the technician will position you appropriately.
- Scanning: The DXA machine consists of a scanning arm that will pass over your body. The technician will operate the machine from a separate control area. During the scan, you need to lie still and breathe normally.
- Area of Examination: The most common areas scanned are the hip and spine, as they are the most indicative of bone health. For the hip scan, your leg may be supported or placed in a brace to rotate the hip slightly. For the spine scan, your legs may be elevated on a cushion to flatten the lower back.
- Duration: The scanning process is usually quick, taking only a few minutes for each area examined. The entire test, including preparation and positioning, typically lasts around 15 to 30 minutes.
- Radiation Exposure: DXA scans involve a very low dose of radiation, much lower than other X-ray procedures. The amount of radiation exposure is considered safe and well below any significant health risks.
- Results: The images obtained from the DXA scan are used to calculate your bone mineral density. The results are usually provided as T-scores and Z-scores. Your doctor will interpret the scores and discuss the findings with you.
It's important to note that the exact procedure may vary slightly depending on the facility and the specific DXA machine used. The test is generally painless and does not require any recovery time, allowing you to resume your normal activities immediately.
What is the Bone Density Testing T score Range?
The T-score is a measure used in bone density testing to compare an individual's bone density to that of a healthy young adult of the same sex. The T-score range is as follows:
- T-score above -1: This range indicates normal bone density. A T-score above -1 means that your bone density is within the range of a healthy young adult.
- T-score between -1 and -2.5: This range indicates low bone density, also known as osteopenia. A T-score between -1 and -2.5 suggests that your bone density is lower than normal but not low enough to be classified as osteoporosis.
- T-score of -2.5 and below: This range indicates osteoporosis. A T-score of -2.5 or lower suggests that your bone density is significantly below the average bone density of a healthy young adult and puts you at a higher risk of fractures.
It's important to note that the T-score provides information about your bone density at the time of the test and does not predict the likelihood of fractures. Other factors, such as age, overall health, and previous fractures, are also important in assessing fracture risk.
Conclusion
In conclusion, bone density testing, specifically dual-energy X-ray absorptiometry (DXA), is a valuable diagnostic tool used to assess bone health and diagnose conditions such as osteoporosis and osteopenia. The T-score, derived from the DXA scan results, provides a standardized measure of an individual's bone density compared to that of a healthy young adult of the same sex.
The T-score range helps classify bone density and guide treatment decisions. A T-score above -1 indicates normal bone density, while a T-score between -1 and -2.5 suggests low bone density or osteopenia. A T-score of -2.5 or lower indicates osteoporosis, characterized by significantly reduced bone density and an increased risk of fractures.
Bone density testing is particularly important for postmenopausal women, men over 70, individuals with specific risk factors, and those already diagnosed with osteoporosis. The results help healthcare providers assess fracture risk, monitor treatment effectiveness, and guide preventive measures or interventions to improve bone health.
It's crucial to remember that bone density testing is just one component of assessing overall bone health. It should be combined with a comprehensive evaluation of individual risk factors, medical history, and lifestyle factors. The interpretation of the T-score and subsequent management decisions should be made in consultation with a healthcare provider who can provide personalized recommendations.
By detecting bone loss early and implementing appropriate interventions, bone density testing plays a vital role in preventing fractures, improving quality of life, and promoting overall skeletal health.









